Bipolar Spectrum Disorder: Definition, Symptoms, Diagnosis, and Treatment Options
What is Bipolar Spectrum Disorder: A brief introduction...
What is Bipolar Spectrum Disorder
Imagine living with intense mood swings that dramatically alter your daily life, relationships, and sense of identity. One day, you’re on top of the world, feeling invincible and filled with boundless energy, only to be followed by a crushing low that leaves you drained and disconnected from the world. This ebb and flow of emotions, marked by episodes of mania, hypomania, and depression, is the lived experience of individuals grappling with Bipolar Spectrum Disorder.
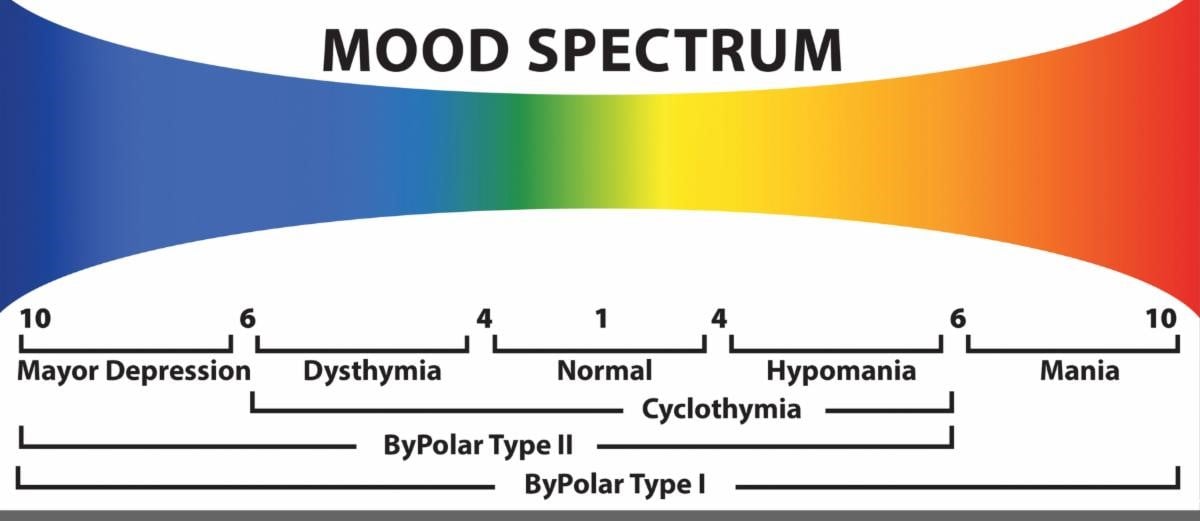
Bipolar Spectrum Disorder (BSD) is a fascinating and complex phenomenon, encompassing a range of interconnected conditions that challenge the traditional notions of mental health and wellness. The term “Bipolar Spectrum” captures the nuances and variability of the condition, implying a gradation of symptoms rather than a fixed diagnosis. This perspective recognizes the individual experiences of patients and underscores the intricate balance between mania, hypomania, depression, and euthymic (stable) states that typify this disorder.
BSD is characterized by the oscillation of mood states, varying in duration, severity, and impact on daily functioning. For instance, individuals with Bipolar I Disorder (BD I) may experience full-blown manic episodes marked by reckless spending, increased risk-taking, or social impulsivity, often leading to substance abuse or addiction. By contrast, those with Bipolar II Disorder (BD II) might encounter milder hypomanic episodes, coupled with more pervasive depressive symptoms, which may not meet the full diagnostic criteria for mania.
Comorbidities are another hallmark of BSD, where multiple health issues converge. Anxiety, substance abuse, feeding disorders, and others often accompany the core bipolar presentation, necessitating integrated treatment strategies. Incorporating key themes and specific attention to comorbidities would ultimately improve long-term outcomes.
We can learn more from Kate’s story: “I’m thirty years old and have Bipolar II Disorder. I typically wake up at six and do a meditation, feeling optimistic and forward-looking. My medications help level out my episodes of severe depression and milder mania. Typically, I exercise or attend to my art. Exercise has helped me not feel confined by one or two feelings of ‘emotions,’ like something could not be what both wanted and felt. Practicing self-care, my moods stabilized and hope returned.”
In BSD, early intervention and continuous medication monitoring can minimize the severity and frequency of episodes. The emotional challenges for these patients are not unlike high winds generating stormy currents, affecting relationships and professional performance, often unseen from the surface. Support that responds more deeply and addresses these problems works better than coping with the storm alone. Using Kate’s story and the exploration of Bipolar Spectrum Disorder yields more than merely psychological insights and is empathetic.
Understanding Bipolar Spectrum Disorder: An expanded overview...
Understanding Bipolar Spectrum Disorder
Bipolar Spectrum Disorder, formerly known as manic-depressive illness, is a complex mental health condition characterized by extreme mood swings that can range from the lows of depression to the highs of mania or hypomania. This condition has been documented for centuries, with ancient Greeks such as Hippocrates and Aretaeus of Cappadocia describing symptoms of the disorder as early as 400 BCE. However, it wasn’t until the late 19th and 20th centuries that the term “bipolar” was introduced, with the first formal diagnostic criteria being established in the 1970s.
So, what exactly is Bipolar Spectrum Disorder? In simple terms, it’s a condition where an individual’s mood and energy levels fluctuate between different emotional states. The four main types of bipolar disorder, which will be discussed in detail later, are bipolar I, bipolar II, cyclothymia, and bipolar disorder not otherwise specified (NOS). According to the National Institute of Mental Health (NIMH), more than 7 million adults in the United States suffer from Bipolar Spectrum Disorder.
One of the most distinctive aspects of Bipolar Spectrum Disorder is its impact on an individual’s emotional state. People with the condition often experience intense feelings of sadness, anger, or hopelessness during depressive episodes, which can last for weeks or even months. On the other hand, manic episodes are marked by elevated mood, increased energy, and a sense of euphoria. This can manifest in impulsive behavior, excessive spending, or reckless decision-making.
Let’s take a look at a case study to illustrate this. Sarah, a successful entrepreneur in her mid-30s, was diagnosed with bipolar I disorder after experiencing a series of intense mood swings. During her manic episodes, Sarah would often stay up all night working on new business ideas, feeling invincible and hyper-focused. However, during her depressive episodes, she would struggle to get out of bed, feeling overwhelmed by her responsibilities and doubting her abilities.
Key Characteristics of Bipolar Spectrum Disorder
- Mood swings: Unpredictable shifts between depressive, manic, or hypomanic episodes, which can last for days, weeks, or even months.
- Emotional intensity: Excessive emotional response to everyday situations, often leading to impulsive behavior or reckless decision-making.
- Energy fluctuations: Significant changes in energy levels, ranging from fatigue during depressive episodes to hyperactivity during manic episodes.
- Sleep disturbances: Difficulty maintaining a regular sleep schedule, which can exacerbate symptoms of Bipolar Spectrum Disorder.
The Four Main Types of Bipolar Disorder
- Bipolar I Disorder: Characterized by at least one manic episode, which may be accompanied by depressive episodes. Bipolar I disorder is the most severe form of the condition.
- Bipolar II Disorder: Defined by at least one major depressive episode and one hypomanic episode. Bipolar II disorder is less severe than bipolar I but can still significantly impact daily life.
- Cyclothymia: A chronic condition marked by periods of hypomania and depression lasting at least two years. Cyclothymia is a milder form of bipolar disorder but can still cause significant distress.
- Bipolar Disorder Not Otherwise Specified (NOS): A diagnosis used when symptoms of bipolar disorder are present but do not fit into the above categories. Bipolar Disorder NOS can manifest in various ways, such as hypomanic episodes without depression or manic episodes with few symptoms.
By understanding the complexities of Bipolar Spectrum Disorder, we can work towards raising awareness and promoting support for individuals and families affected by this condition. In the next section, we’ll explore the signs and symptoms of bipolar disorder in greater detail, including warning signs, common comorbidities, and long-term effects on physical and mental health.
Related Terms and Concepts:
As we delve deeper into the complexities of Bipolar Spectrum Disorder (BSD), it’s essential to understand the various related terms and concepts that can impact diagnosis, treatment, and overall quality of life.
Mood Episodes: Distinct periods of abnormally elevated or depressed mood, manifesting as manic, hypomanic, depressive, or mixed states.
Cyclical Patterns: Predictable sequences of mood episodes, assisting individuals and professionals in anticipating future episodes.
Mixed Features: The co-occurrence of manic and depressive symptoms within a single episode, making diagnosis more challenging.
Comorbidities: The presence of one or more additional mental health conditions, such as anxiety or ADHD, alongside BSD.
Stress and Trigger Management: Learning to manage triggers can help reduce mood episode frequency and severity.
Sleep Hygiene: Establishing a consistent sleep schedule to improve sleep quality.
Mindfulness and Self-Care: Practices like meditation and journaling to enhance emotional regulation.
Family History and Genetic Predisposition: Understanding genetic risks can inform treatment and early intervention strategies.
Therapeutic Alliance: A strong relationship with healthcare providers enhances treatment outcomes.
Recovery-Oriented Approach: Focusing on individual goals and needs fosters empowerment and resilience.
By understanding these related terms and concepts, individuals with BSD, their loved ones, and healthcare providers, can work together for improved outcomes.
Examples and Case Studies: Concrete examples exploring how Bipolar Spectrum Disorder is applied in practice.
Understanding Bipolar Spectrum Disorder can be complex, but exploring real-life examples and case studies provides valuable insights. Here are some illustrations that demonstrate how this disorder manifests:
Case Study 1: Alex’s Struggle with Cyclothymia
Alex, a 32-year-old graphic designer, experienced persistent mood swings lasting at least two years, including mild depression interspersed with brief episodes of elevated mood. Their struggles presented challenges in diagnosis.
Case Study 2: Jamie’s Bipolar I Diagnosis
Jamie, a 25-year-old college student, experienced sudden mania leading to impulsivity and reckless behavior, highlighting the importance of accurate diagnosis.
Example: Mood-Swinging Athletes
Bipolar Spectrum Disorder can also affect athletes who might face extreme mood swings due to performance pressures.
Case Study 3: Rachel’s Misdiagnosis and Treatment
Rachel, a 40-year-old entrepreneur, initially misdiagnosed with Unipolar Depression, was correctly diagnosed and received effective treatment after her clinicians reassessed her symptoms.
Illustration: Bipolar Spectrum Disorder in the Arts
Bipolar Spectrum Disorder has been associated with creativity, as exemplified by Vincent van Gogh's emotional turmoil, which highlights the importance of recognizing these connections.
By analyzing these examples, we gain a nuanced understanding of Bipolar Spectrum Disorder, emphasizing the need for accurate diagnosis, effective treatment, and compassionate support.
Diagnosis and Treatment: Understanding how Bipolar Spectrum Disorder is diagnosed and treated.
Living with Bipolar Spectrum Disorder can be unpredictable and overwhelming. Accurate diagnosis is crucial for effective management.
The diagnosis involves a combination of clinical interviews, psychological evaluations, and communication with family members, using tools like the DSM-5 for standardized criteria.
Initial Assessment: In-depth interviews gather background information.
Diagnostic Interview: Evaluation scales confirm symptoms and assess various behaviors.
Laboratory Tests: Tests to rule out other medical conditions.
A comprehensive diagnosis enables a personalized treatment plan centered on medication and psychotherapy.
Key Components of Bipolar Spectrum Disorder: Key components unpacked.
Bipolar Spectrum Disorder comprises interconnected components that vary in severity. Understanding these can aid in compassionate treatment approaches.
1. Mood Episodes: Characterized by manic, hypomanic, or depressive experiences.
2. Cognitive Distortions: Patterns amplifying symptoms.
3. Emotional Dysregulation: Challenges managing emotions.
4. Impulsivity: Acting without contemplation, leading to risky behavior.
By recognizing these components, we can foster informed and supportive environments for those affected by Bipolar Spectrum Disorder.
Living with Bipolar Spectrum Disorder: Tips and advice.
Receiving a diagnosis can transform life experiences, but effective strategies exist for support.
1. Develop a Treatment Plan: Collaborate with professionals for tailored strategies, including therapy and medication.
2. Prioritize Self-Care: Incorporate mindfulness, exercise, and healthy habits.
3. Build a Support Network: Connect with others for shared experiences and accountability.
Incorporating these tips can enhance the quality of life for those living with Bipolar Spectrum Disorder. For additional resources on anxiety and ADHD support, consider utilizing tools from GoblinX, available on our mobile app, to find effective coping strategies.