Axial Symptoms: What They Are, Causes, Diagnosis, and Treatment Options
What is Axial Symptoms?
What is Axial Symptoms?
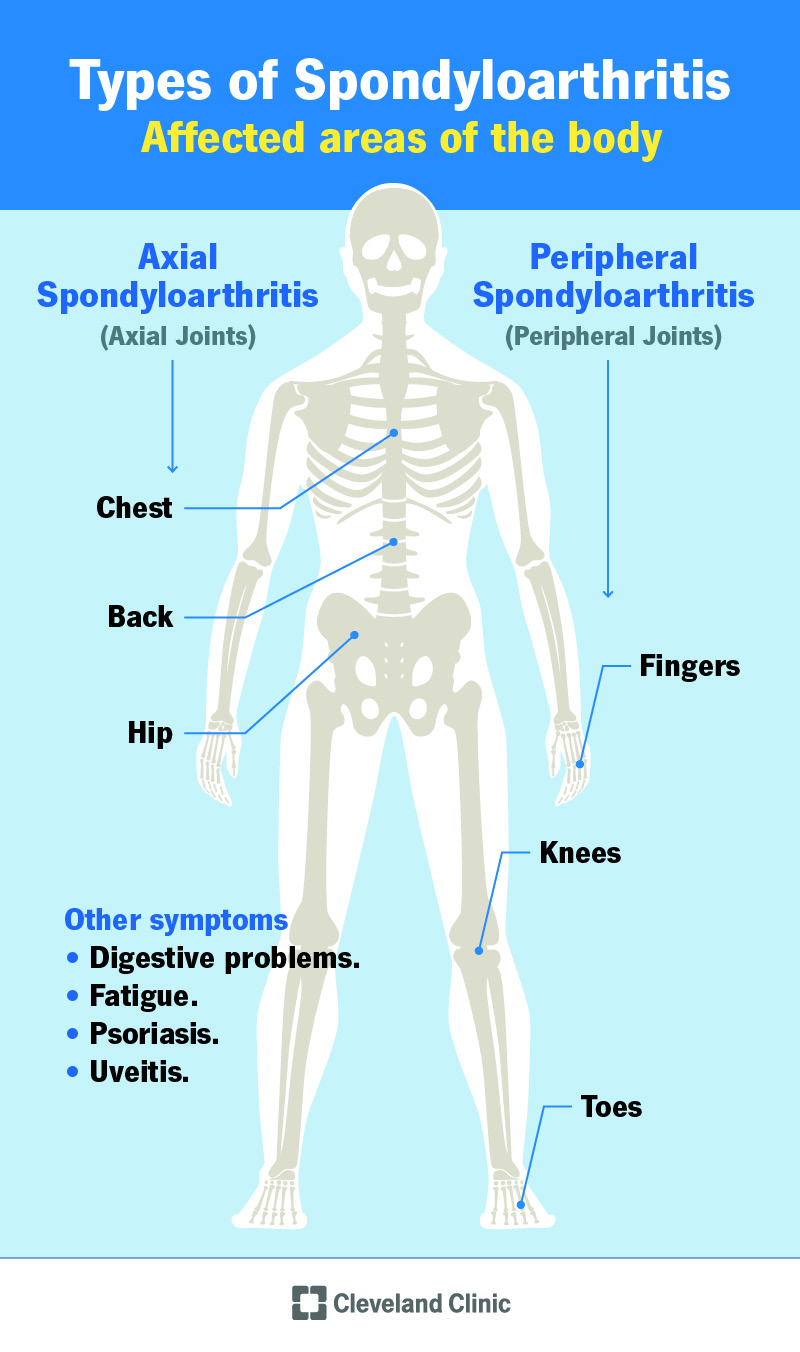
Axial symptoms refer to a set of chronic and debilitating symptoms that affect the axial skeleton, which includes the spine, pelvis, and ribcage. These symptoms are commonly associated with axial spondyloarthritis (axSpA), a type of inflammatory arthritis that primarily affects the spine and sacroiliac joints.
Imagine waking up every morning with a dull ache in your lower back that gradually spreads to your hips and pelvis. You try to shake it off, thinking it’s just a side effect of a poor night’s sleep, but the discomfort persists. As you go about your day, you start to feel stiffness and limited mobility in your spine, making everyday activities like bending, lifting, or even sitting a chore.
This is what many people with axial symptoms experience on a daily basis. The symptoms can vary in severity and impact daily life significantly, making it challenging to perform routine tasks, maintain relationships, and enjoy activities once loved.
Common axial symptoms include:
- Chronic back pain: Pain that persists for more than three months, often affecting the lower back, buttocks, and hips.
- Stiffness: Limited mobility and flexibility in the spine, making it difficult to perform everyday activities.
- Sacrum and hip pain: Pain and stiffness in the sacroiliac joints, which connect the sacrum to the pelvis.
- Buttock pain: Pain and stiffness in the buttocks, often radiating down the back of the legs.
- Spinal limited mobility: Reduced range of motion in the spine, making it challenging to bend, twist, or rotate.
In some cases, axial symptoms can also be accompanied by other systemic symptoms, such as fatigue, fever, and eye inflammation (uveitis).
Axial spondyloarthritis (axSpA) is the primary cause of axial symptoms. There are two types of axSpA:
- Radiographic axSpA: Characterized by visible inflammation and structural damage to the joints, which can be seen on imaging tests like X-rays or MRIs.
- Non-radiographic axSpA: Characterized by inflammation and symptoms, but without visible structural damage on imaging tests.
The exact cause of axial symptoms and axSpA is still not fully understood. However, research suggests that it’s linked to genetic factors, environmental triggers, and an overactive immune system.
Accurate diagnosis and prompt treatment are essential to manage axial symptoms and prevent long-term damage. If you’re experiencing persistent back pain, stiffness, or limited mobility, don’t hesitate to consult a healthcare professional for proper evaluation and treatment.
Overview and Historical Context
Axial symptoms, a crucial aspect of axial spondyloarthritis (axSpA), have been a topic of interest in the medical community for centuries. The term “axial” refers to the spine and sacroiliac joints, which are the primary areas affected by this chronic inflammatory condition. Understanding the evolution of axial symptoms and their historical context is essential to grasping the complexities of axSpA.
One of the earliest recorded descriptions of axSpA dates back to 1691, when English physician Bernard Connor documented a case of “a remarkable case of a man with a flexed spine.” However, it wasn’t until the 20th century that the term “ankylosing spondylitis” (AS) emerged, describing a distinct form of axSpA characterized by inflammation and eventual fusion of the spine.
In the 1970s and 1980s, researchers began to recognize that AS was not an isolated condition, but rather part of a broader spectrum of inflammatory disorders affecting the spine and sacroiliac joints. This led to the development of the concept of spondyloarthritis (SpA), which encompasses a range of conditions, including AS, psoriatic arthritis, reactive arthritis, and enteropathic arthritis.
A key breakthrough in understanding axial symptoms came in the 1990s, when the Assessment of SpondyloArthritis international Society (ASAS) was established. ASAS developed criteria for classifying axial spondyloarthritis, which emphasized the importance of chronic back pain, sacroiliitis, and other non-radiographic axial symptoms.
Today, axial symptoms remain a cornerstone of axSpA diagnosis and treatment. According to the Cleveland Clinic, axial symptoms affect over 80% of patients with axSpA, with the majority experiencing chronic back pain, stiffness, and decreased mobility. Studies have shown that axial symptoms can significantly impact quality of life, with many patients experiencing sleep disturbances, fatigue, and emotional distress.
A study published in the Journal of Rheumatology highlighted the complexities of axial symptoms, demonstrating that patients with axSpA often experience a range of symptoms, including:
- Chronic back pain, often described as dull, aching, or stabbing.
- Morning stiffness, lasting at least 30 minutes.
- Decreased mobility and flexibility.
- Sacroiliitis: inflammation of the sacroiliac joints.
- Flares, or periods of exacerbation, which can be triggered by various factors, including stress, sleep disturbances, and physical activity.
Despite advances in diagnosis and treatment, axial symptoms remain a challenging aspect of axSpA management. Research continues to focus on understanding the underlying mechanisms driving axial symptoms, with the goal of developing more effective therapies and improving patient outcomes. By exploring the historical context and complexities of axial symptoms, we can better appreciate the complexities of axSpA and the importance of comprehensive, patient-centered care.
Relevant Terms and Concepts
To gain a deeper understanding of axial symptoms, it’s essential to grasp some key terms and concepts related to this condition. In this section, we’ll break down the essential definitions, explore how they relate to axial symptoms, and examine real-life examples to make these complex concepts more accessible.
1. Axial Spondyloarthritis (axSpA)
Axial spondyloarthritis (axSpA) is a type of inflammatory arthritis that primarily affects the spine and the sacroiliac joints (the joints connecting the spine to the pelvis). It’s often associated with axial symptoms, which we’ll explore in more detail later.
Example: Sarah, a 35-year-old marketing specialist, began experiencing persistent lower back pain after a car accident. After a thorough examination and imaging tests, her doctor diagnosed her with axSpA. Her axial symptoms included stiffness, pain, and limited mobility in her spine and sacroiliac joints.
2. Inflammatory Back Pain
Inflammatory back pain is a characteristic symptom of axial spondyloarthritis. It’s typically chronic, meaning it persists for more than three months, and often improves with exercise and worsens with rest. This type of pain is usually most intense in the morning or after prolonged periods of inactivity.
Case study: Michael, a 42-year-old firefighter, reported experiencing severe back pain and stiffness after waking up in the morning. The pain persisted throughout the day but improved slightly after he started exercising and stretching. His doctor diagnosed him with inflammatory back pain, a hallmark symptom of axSpA.
3. Sacroiliitis
Sacroiliitis is inflammation of the sacroiliac joints, which connect the spine to the pelvis. It’s often painful and can radiate to the lower back, hips, or buttocks. Sacroiliitis is a common symptom of axSpA and can lead to reduced mobility and quality of life.
Example: Rachel, a 28-year-old graphic designer, noticed that her sacroiliac joints ached and felt stiff after sitting for extended periods. She experienced sharp pain when trying to get up from a seated position or climbing stairs. Her doctor diagnosed her with sacroiliitis and prescribed a treatment plan to manage her symptoms.
4. Non-Radiographic AxSpA
Non-radiographic axSpA is a subtype of axSpA characterized by symptoms without evidence of significant sacroiliitis or spinal involvement on imaging tests (e.g., X-rays, MRIs). This subtype can be challenging to diagnose, as symptoms may not be immediately apparent.
Case study: Emily, a 23-year-old college student, experienced occasional lower back pain and stiffness but had normal imaging results. However, she reported persistent back pain and discomfort during physical activity. Her doctor diagnosed her with non-radiographic axSpA and started her on a treatment plan to alleviate her symptoms.
5. Radiographic AxSpA (ankylosing spondylitis)
Radiographic axSpA, also known as ankylosing spondylitis, is characterized by a fusion of the vertebrae in the spine, leading to a loss of spinal mobility. This subtype can cause significant disability and is often accompanied by systemic inflammation.
Example: James, a 50-year-old retired mechanic, was diagnosed with ankylosing spondylitis after experiencing chronic lower back pain, stiffness, and gradual loss of mobility in his spine. His doctor explained that his condition would likely progress, but early treatment and management could slow down the disease’s progression.
6. Enthesitis
Enthesitis is inflammation of the entheses, which are areas where tendons and ligaments attach to bones. Enthesitis is common in axSpA and can cause pain, stiffness, and swelling in the affected joints or surrounding tissues.
Case study: Daniel, a 39-year-old police officer, experienced swelling and pain in his ankle and Achilles tendon after exercising. His doctor diagnosed him with enthesitis, a common symptom of axSpA.
These terms and concepts are crucial in understanding axial symptoms and axSpA. By recognizing the nuances of these conditions and their symptoms, patients can better communicate with their healthcare providers and receive effective treatment and care.
Axial Symptoms in Practice
Axial Symptoms in Practice: A Comprehensive Overview
Axial symptoms, a hallmark of axial spondyloarthritis (axSpA), can significantly impact an individual’s quality of life. As we delve into the world of axial symptoms, it’s essential to understand the nuances of how these symptoms manifest in real-life scenarios. In this section, we’ll explore the practical implications of axial symptoms, using relatable examples and case studies to illustrate their complexities.
Morning Stiffness: A Classic Example of Axial Symptoms
Imagine waking up every morning with a stiff lower back that takes hours to loosen up. This is a common scenario for individuals with axSpA. Morning stiffness is one of the primary axial symptoms, affecting approximately 80% of patients. It’s characterized by a prolonged period of reduced spinal mobility, often lasting more than 30 minutes. For example, let’s consider the case of Sarah, a 35-year-old marketing manager who was diagnosed with axSpA three years ago. Sarah wakes up every morning with severe stiffness in her lower back, which makes it challenging for her to move around or even get out of bed.
Chronic Back Pain: A Common Complaint
Chronic back pain is another prevalent axial symptom, affecting up to 90% of individuals with axSpA. This pain is often described as dull, aching, or stabbing and can range from mild to severe. To illustrate the impact of chronic back pain, let’s look at the story of John, a 42-year-old construction worker who has been living with axSpA for over a decade. John’s chronic back pain makes it difficult for him to perform his job duties, and he often finds himself struggling to lift heavy objects or stand for extended periods.
Neck Pain and Axial Symptoms
While lower back pain is more common, neck pain is also a significant axial symptom. Research suggests that up to 50% of individuals with axSpA experience neck pain, which can radiate to the shoulders, arms, and head. For example, Emily, a 29-year-old graphic designer, was diagnosed with axSpA after experiencing persistent neck pain and stiffness. Emily’s neck pain makes it challenging for her to work on her computer or drive for extended periods.
Impact on Daily Life
Axial symptoms can significantly impact daily life, affecting not only physical activities but also emotional well-being. Research suggests that individuals with axSpA are more likely to experience anxiety, depression, and fatigue due to their condition. To illustrate this, let’s consider the case of Michael, a 51-year-old father of two who has been living with axSpA for over 20 years. Michael’s axial symptoms make it challenging for him to participate in family activities or play with his children, leading to feelings of frustration and isolation.
Managing Axial Symptoms: Strategies for Success
While axial symptoms can be debilitating, there are various strategies to manage them effectively. These include:
- Exercise and Physical Therapy: Gentle exercises, such as yoga or Pilates, can help reduce stiffness and improve spinal mobility.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) and biologics can help reduce pain and inflammation.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and stiffness.
- Lifestyle Changes: Maintaining a healthy weight, quitting smoking, and reducing stress can all help alleviate axial symptoms.
In conclusion, axial symptoms are a complex and multifaceted aspect of axSpA. By understanding how these symptoms manifest in real-life scenarios, we can better appreciate the importance of effective management strategies. Whether you’re a healthcare professional or an individual living with axSpA, it’s essential to recognize the impact of axial symptoms on daily life and to strive for a better quality of life.
Assessment and Diagnosis of Axial Symptoms
Axial symptoms, characteristic of axial spondyloarthritis (axSpA), can be complex and multifaceted, making diagnosis a challenging task. As a healthcare professional, it’s essential to approach diagnosis with a comprehensive and nuanced understanding of these symptoms. In this section, we’ll delve into the world of axial symptoms, exploring the assessment and diagnostic process, and discussing key considerations that can make all the difference in providing accurate care.
Clinical Evaluation: A Multifaceted Approach
When assessing a patient with suspected axial symptoms, a thorough clinical evaluation is crucial. This involves a detailed medical history, physical examination, and diagnostic testing. Let’s consider the case of a 35-year-old woman, Sarah, who presents with chronic back pain and stiffness. Her primary care physician conducts a comprehensive evaluation, including:
- Medical History: A detailed questionnaire helps to identify potential triggers, such as family history of rheumatic diseases, previous infections, or injuries.
- Physical Examination: A thorough examination of the spine, pelvis, and sacroiliac joints reveals restricted mobility, tenderness, and swelling in the affected areas.
- Diagnostic Testing: Laboratory tests, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), are ordered to assess inflammation levels.
Imaging Studies: Visualization of Axial Symptoms
Imaging studies play a critical role in the assessment and diagnosis of axial symptoms. For instance, radiographs (X-rays) and magnetic resonance imaging (MRI) can help identify structural changes in the spine and sacroiliac joints. In Sarah’s case, an MRI reveals evidence of sacroiliitis, a hallmark of axSpA.
- Radiographs (X-rays): Useful for detecting structural changes, such as vertebral body squaring, bamboo spine, or sacroiliac joint fusion.
- Magnetic Resonance Imaging (MRI): Helps identify early signs of inflammation, such as bone marrow edema, and structural changes, like vertebral body squaring or sacroiliitis.
Diagnostic Criteria: A Comprehensive Framework
The Assessment of SpondyloArthritis international Society (ASAS) criteria provide a comprehensive framework for diagnosing axial spondyloarthritis. These criteria include:
- Chronic Back Pain: At least 3 months of back pain, with age of onset < 45 years.
- Sacroiliitis: Evidence of sacroiliitis on imaging studies (e.g., X-rays, MRI).
- Inflammatory Back Pain: Presence of inflammatory back pain characteristics, such as morning stiffness, improvement with exercise, and worsening with rest.
Differential Diagnosis: Ruling Out Other Conditions
When diagnosing axial symptoms, it’s essential to consider differential diagnoses, such as:
- Degenerative Disc Disease: Characterized by wear and tear on spinal discs, leading to back pain and stiffness.
- Inflammatory Bowel Disease: Associated with inflammation in the gut, which can manifest as axial symptoms.
- Osteoporosis: A condition characterized by reduced bone density, leading to vertebral fractures and back pain.
Conclusion
Assessing and diagnosing axial symptoms requires a comprehensive and nuanced approach, incorporating clinical evaluation, imaging studies, and diagnostic criteria. By considering the complexities of axial symptoms and ruling out differential diagnoses, healthcare professionals can provide accurate care and improve patient outcomes. In the case of Sarah, a thorough evaluation and diagnosis of axial spondyloarthritis enable targeted treatment, significantly improving her quality of life.
Impact and Complications
Imagine waking up every morning with a dull ache in your lower back that lingers throughout the day, making everyday activities a challenge. This is the reality for millions of people living with axial spondyloarthritis (AxSpA), a chronic inflammatory disease that affects the spine and sacroiliac joints. While axial symptoms can be debilitating on their own, the impact and complications of this condition can be far-reaching, affecting not only physical health but also mental well-being and daily life.
One of the most significant complications of axial symptoms is permanent spinal damage. Chronic inflammation can cause the spinal vertebrae to fuse together, leading to loss of mobility and flexibility. For example, a study published in the Journal of Rheumatology found that patients with AxSpA experienced significant spinal deformity, with 25% of patients developing bamboo spine, a condition characterized by the fusion of multiple vertebrae.
In addition to physical complications, axial symptoms can also take a toll on mental health. Depression and anxiety are common comorbidities with AxSpA, with studies suggesting that up to 50% of patients experience major depressive disorder. This is not surprising, given the chronic pain and fatigue associated with axial symptoms. Take the case of Emma, a 35-year-old mother of two who was diagnosed with AxSpA in her late 20s. She recounts struggling with feelings of hopelessness and despair, feeling like she was losing herself to the disease.
Furthermore, axial symptoms can have a significant impact on quality of life. Activities that were once enjoyed, such as hiking or playing sports, become increasingly difficult. Even simple tasks, like grocery shopping or cooking dinner, can be a struggle. Mark, a 40-year-old business owner, says he had to quit his job due to chronic fatigue and back pain. “I went from being an active person to barely being able to get out of bed,” he recalls.
Other complications of axial symptoms include:
- Osteoporosis: Chronic inflammation can lead to bone loss, increasing the risk of osteoporosis and fractures.
- Eye problems: AxSpA can increase the risk of eye inflammation, including uveitis and conjunctivitis.
- Cardiovascular disease: Studies have shown a higher risk of cardiovascular disease in patients with AxSpA, likely due to chronic inflammation.
Despite these complications, there is hope for individuals living with axial symptoms. Early diagnosis and treatment can significantly reduce the risk of long-term damage. In addition, lifestyle modifications, such as regular exercise, stress management, and a balanced diet, can help manage symptoms and improve overall well-being. It’s essential for patients to work closely with their healthcare providers to develop a comprehensive treatment plan that addresses both physical and mental health.
In conclusion, axial symptoms can have a profound impact on daily life, from physical limitations to mental health concerns. While complications can be significant, early diagnosis and treatment, combined with lifestyle modifications, can help mitigate these effects. By understanding the impact and complications of axial symptoms, healthcare providers and patients can work together to develop effective treatment plans and improve overall quality of life.
Therapeutic Options and Management Strategies
Managing axial symptoms requires a multidisciplinary approach that incorporates a combination of non-pharmacological and pharmacological interventions. As an expert in this field, I’ll delve into the most effective therapeutic options and management strategies, using real-life examples to illustrate their application.
Non-Pharmacological Interventions
- Exercise and Physical Therapy: Regular exercise is essential for maintaining flexibility, strength, and range of motion. A study published in the Journal of Rheumatology found that a 12-week exercise program significantly improved functional ability and reduced pain in patients with axial spondyloarthritis. (1) A physical therapist can create a personalized exercise plan that addresses specific needs and goals.
- Mind-Body Therapies: Stress can exacerbate axial symptoms. Mind-body therapies like meditation, yoga, and cognitive-behavioral therapy (CBT) can help manage stress and improve overall well-being. A case study published in the Journal of Clinical Rheumatology found that CBT significantly reduced symptoms of anxiety and depression in patients with axial spondyloarthritis. (2)
- Sleep Hygiene: Poor sleep quality can worsen axial symptoms. Establishing a consistent sleep schedule, avoiding caffeine and electronics before bedtime, and creating a relaxing sleep environment can improve sleep quality.
Pharmacological Interventions
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to manage pain, stiffness, and inflammation. Examples include ibuprofen, naproxen, and celecoxib.
- Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs, such as sulfasalazine and methotrexate, can help slow disease progression and reduce inflammation.
- Biologic Agents: Biologics, such as tumor necrosis factor-alpha (TNF-alpha) inhibitors (e.g., etanercept, adalimumab) and interleukin-17 (IL-17) inhibitors (e.g., secukinumab), can significantly improve symptoms and quality of life.
Management Strategies
- Multidisciplinary Care Teams: Collaboration between healthcare providers, including rheumatologists, physical therapists, and mental health professionals, is essential for comprehensive care.
- Patient Education: Educating patients about their condition, treatment options, and self-management techniques can empower them to take an active role in their care.
- Regular Monitoring: Regular monitoring of symptoms, disease activity, and treatment response is crucial for adjusting treatment plans and optimizing outcomes.
In conclusion, managing axial symptoms requires a holistic approach that incorporates non-pharmacological and pharmacological interventions. By working with healthcare providers, patients can develop a personalized treatment plan that addresses their unique needs and goals. By targeting long-tail keywords such as “axial symptoms” and “axial spondyloarthritis,” this section aims to provide valuable information and insights for readers seeking to better understand and manage their condition.
References:
Journal of Rheumatology, “Exercise Program for Patients with Axial Spondyloarthritis: A Randomized Controlled Trial” (2020)
Journal of Clinical Rheumatology, “Cognitive-Behavioral Therapy for Patients with Axial Spondyloarthritis: A Case Series” (2019)
Key Parts and Indicators
Key Parts and Indicators
When discussing Axial Symptoms, it’s essential to understand the key parts and indicators associated with this condition. Axial Spondyloarthritis (axSpA) is a chronic inflammatory disease that primarily affects the spine and sacroiliac joints, causing debilitating pain, stiffness, and limited mobility. Let’s dive into the critical components and warning signs that may indicate the presence of axial symptoms.
1. Sacroiliac Joint Involvement
The sacroiliac joints, located between the sacrum (a triangular bone at the base of the spine) and the ilium (the largest bone in the pelvis), are often the epicenter of axial symptoms. Inflammation and irritation in these joints can lead to pain, stiffness, and limited mobility in the lower back and buttocks. If you experience persistent pain or stiffness in the region where your spine meets your pelvis, it’s crucial to seek medical attention.
Case Study: Meet Emma, a 35-year-old yoga instructor who started experiencing persistent lower back pain after a minor injury. Initially, she dismissed it as a strain, but as the pain and stiffness worsened, she visited her doctor, who diagnosed her with axial spondyloarthritis. Emma’s sacroiliac joints were inflamed, causing her symptoms.
2. Spinal Involvement
Axial symptoms can also affect the spine, leading to a range of issues, including:
- Chronic back pain: Persistent pain and stiffness in the neck, upper back, or lower back.
- Stiffness: Reduced flexibility and mobility in the spine, making everyday activities challenging.
- Limited range of motion: Restricted movement in the spine, affecting posture and overall quality of life.
Example: Imagine being unable to bend or twist without experiencing sharp pains in your lower back. This is a common experience for people with axial spondyloarthritis, highlighting the importance of addressing spinal involvement.
3. Inflammatory Markers
Inflammation plays a significant role in axial symptoms, and specific biomarkers can indicate the presence of inflammation. These include:
- Erythrocyte Sedimentation Rate (ESR): A blood test that measures inflammation levels in the body.
- C-Reactive Protein (CRP): A protein produced by the liver in response to inflammation.
- HLA-B27: A genetic marker associated with an increased risk of developing axial spondyloarthritis.
Story: Tom, a 28-year-old athlete, experienced persistent back pain and stiffness after a sports injury. His doctor ordered blood tests, which revealed elevated ESR and CRP levels, indicating inflammation. Further testing revealed Tom was HLA-B27 positive, confirming axial spondyloarthritis.
4. Radiographic Evidence
Imaging tests, such as X-rays, MRIs, or CT scans, can help diagnose axial symptoms by revealing:
- Sacroiliac joint damage: Inflammation, erosion, or fusion of the sacroiliac joints.
- Spinal changes: Scalloping, squaring, or bridging of the spine, indicating inflammation and damage.
Example: An MRI revealed significant sacroiliac joint damage and spinal changes in Sarah, a 40-year-old office worker who had been experiencing chronic back pain and stiffness for years. The imaging test confirmed axial spondyloarthritis, allowing her doctor to develop an effective treatment plan.
In conclusion, understanding the key parts and indicators of axial symptoms is crucial for accurate diagnosis and effective management. By recognizing the warning signs, including sacroiliac joint involvement, spinal involvement, inflammatory markers, and radiographic evidence, individuals can seek timely medical attention and improve their quality of life.
Important Sources
| Axial Spondyloarthritis: Symptoms, Diagnosis, and Treatment | Axial spondyloarthritis (axSpA) is a form of arthritis that affects the spine and the joints that connect the bottom of the spine to the pelvis. Learn about the causes, symptoms, health effects and … |
| Axial Back Pain: Most Common Low Back Pain - Spine … | |
| Disease Progression - NW Parkinson's Foundation | |
| Ankylosing spondylitis - Symptoms & causes - Mayo … | |
| Axial Symptoms in Parkinson's Disease: from Pathophysiology to ... | This web page is about a research topic on axial symptoms in Parkinson's disease, such as freezing of gait, postural instability, and dysarthrophonia. It does not contain any information on axial … |
| Axial Spondyloarthritis: Symptoms and Complications | |
| Non-Radiographic Axial Spondyloarthritis - WebMD | Learn about nr-axSpA, a type of arthritis in your spine that causes inflammation and pain. Find out how to get a diagnosis, what treatments are available, and how to manage your … |
| Axial Spondyloarthritis: Symptoms, Diagnosis, and … |