Understanding the Connection Between ADHD and Drinking: Managing Co-occurring Issues
Key Takeaways
| Statistic/Fact | Description |
|---|---|
| 30-50% of ADHD individuals have a co-occurring addiction | Research suggests a strong connection between ADHD and alcohol/substance use disorders |
| Higher risk of binge drinking in ADHD individuals | Studies show that individuals with ADHD are more likely to engage in heavy drinking and binge drinking |
| Inhibitory control deficits linked to alcohol use in ADHD | Individuals with ADHD often struggle with impulsivity and self-regulation, increasing the risk of excessive drinking |
| Early substance use exposure can exacerbate ADHD symptoms | Research indicates that early exposure to substances can worsen ADHD symptoms and impair treatment response |
| Comorbid substance use disorders affect treatment outcomes and ADHD symptom severity | Accurate diagnosis and treatment of co-occurring substance use disorders is crucial for effective ADHD management |
| Physiological mechanisms behind ADHD and substance use overlap, including reward system dysregulation | Shared underlying neurobiological mechanisms contribute to the development of comorbid ADHD and substance use disorders |
| Individuals with ADHD-related substance use disorders may require specialized treatment approaches | Tailored interventions addressing ADHD-specific needs can improve treatment outcomes and reduce substance use |
| Parental ADHD is a risk factor for offspring alcohol use and related problems | Hereditary factors contribute to the development of ADHD and substance use disorders in offspring |
| Siblings of individuals with ADHD have an increased risk of developing substance use disorders | Family history of ADHD and substance use disorders increases an individual's risk of developing a co-occurring substance use disorder |
How Alcohol Affects Those with ADHD: Understanding the Risks
Title: The Hidden Dangers of ADHD and Drinking: How Alcohol Impacts ADHD Symptoms and Treatment
Summary: For individuals with Attention Deficit Hyperactivity Disorder (ADHD), the decision to drink alcohol can have far-reaching consequences on their symptoms, treatment, and overall well-being. Research suggests that alcohol use can exacerbate ADHD symptoms, interact negatively with medications, and increase the risk of depression and addiction. Alcohol can also mask ADHD symptoms in the short-term, leading to delayed diagnosis and treatment. In this article, we’ll delve into the risks associated with ADHD and drinking, including the impact on ADHD symptoms, medication efficacy, and mental health. By understanding these risks, individuals with ADHD can make informed decisions about their drinking habits and create a healthier, more balanced lifestyle.
Optimized Keywords: ADHD and drinking, ADHD symptoms and alcohol, ADHD medication and alcohol interactions, ADHD and depression, ADHD addiction risks.
Meta Description: Discover how alcohol can worsen ADHD symptoms, interfere with medication, and increase depression and addiction risks. Learn how to make informed decisions about drinking and manage ADHD effectively.
Header Tags: H1 - The Hidden Dangers of ADHD and Drinking, H2 - How Alcohol Affects ADHD Symptoms, H3 - Interactions with ADHD Medication, H4 - Increased Risk of Depression and Addiction.

The Link Between ADHD and Alcohol Use Disorder: What’s the Connection?
Individuals with Attention Deficit Hyperactivity Disorder (ADHD) are at a higher risk of developing Alcohol Use Disorder (AUD), a condition characterized by compulsive and excessive drinking. Research suggests that the relationship between ADHD and AUD is bidirectional, meaning that each condition can increase the risk of developing the other. In this article, we will explore the complex connection between ADHD and drinking, and what it means for individuals with ADHD who struggle with alcohol use.
The ADHD-AUD Connection: A Bidirectional Relationship
Studies have consistently shown that individuals with ADHD are more likely to develop AUD, with one meta-analysis suggesting that the prevalence of AUD is two times higher in adults with ADHD compared to the general population. Conversely, research has also found that individuals with AUD are more likely to experience ADHD symptoms, with one study estimating that up to 70% of individuals with AUD also meet the criteria for ADHD.
How ADHD Increases the Risk of Developing AUD
Several factors contribute to the increased risk of developing AUD in individuals with ADHD, including:
- Impulsivity: Individuals with ADHD are more likely to engage in impulsive behaviors, including substance use, which can lead to the development of AUD.
- Comorbid Externalizing Psychological Symptoms: Individuals with ADHD are more likely to experience comorbid externalizing symptoms, such as conduct disorder or oppositional defiant disorder, which can increase the risk of developing AUD.
- Neurotransmitter Imbalance: ADHD is associated with an imbalance of neurotransmitters, including dopamine and norepinephrine, which play a role in the development and maintenance of AUD.
- Coping Mechanism: Individuals with ADHD may turn to alcohol as a coping mechanism for stress, anxiety, or other emotions, which can lead to the development of AUD.
How AUD Increases the Risk of ADHD-like Symptoms
Conversely, research has also found that AUD can increase the risk of ADHD-like symptoms, including:
- Cognitive Impairment: Chronic alcohol use can lead to cognitive impairment, including attention and memory deficits, which are similar to the cognitive symptoms experienced by individuals with ADHD.
- Executive Function Deficits: Alcohol use can impair executive function skills, including planning, organization, and self-regulation, which are often impaired in individuals with ADHD.
- Emotional Dysregulation: AUD is associated with emotional dysregulation, including increased anxiety and depression, which can exacerbate ADHD symptoms.
Breaking the Cycle: Treatment and Support for Individuals with ADHD and AUD
Breaking the cycle of addiction and ADHD requires a comprehensive treatment plan that addresses both conditions simultaneously. Strategies for individuals with ADHD and AUD include:
- Medication Management: Medications, such as stimulants and non-stimulants, can help manage ADHD symptoms, while medications, such as benzodiazepines and non-benzodiazepines, can help manage AUD symptoms.
- Cognitive-Behavioral Therapy: Cognitive-behavioral therapy (CBT) can help individuals with ADHD and AUD identify and change negative thought patterns and behaviors that contribute to substance use.
- Behavioral Interventions: Behavioral interventions, such as contingency management and motivational interviewing, can help individuals with ADHD and AUD develop healthier coping mechanisms and reduce substance use.
- Support Groups: Support groups, such as Alcoholics Anonymous and Adfam, can provide individuals with ADHD and AUD with a sense of community and support as they work through their recovery.
In conclusion, the link between ADHD and AUD is complex and bidirectional, with each condition increasing the risk of developing the other. By understanding the factors that contribute to the ADHD-AUD connection, individuals with ADHD and AUD can develop treatment plans that address both conditions simultaneously, leading to improved outcomes and reduced risk of relapse.
ADHD and Alcohol: Increased Symptoms and Risk of Addiction
Individuals with Attention Deficit Hyperactivity Disorder (ADHD) are more susceptible to experiencing increased symptoms and a higher risk of addiction when consuming alcohol. While occasional drinking may not seem to have a significant impact, regular consumption can lead to a significant deterioration in ADHD symptoms, particularly insomnia, and increase the likelihood of developing an addiction.
ADHD and Alcohol Interaction
Alcohol’s interaction with the brain’s neurotransmitters can exacerbate symptoms of ADHD, including:
- Increased impulsivity: Alcohol can impair judgment and lead to impulsive behaviors, making it difficult for individuals with ADHD to control their impulses.
- Worsened attention deficit: Alcohol’s effects on the brain can worsen attention deficit symptoms, making it challenging to focus and stay on task.
- Heightened anxiety and stress: Alcohol’s stimulant effects can contribute to increased anxiety and stress levels, which can be particularly problematic for individuals with ADHD who often experience anxiety and stressors.
Insomnia and ADHD
The relationship between insomnia and ADHD is complex. Research suggests that individuals with ADHD are more likely to experience insomnia, and that alcohol can further exacerbate this symptom. Drinking alcohol can disrupt sleep patterns, leading to lighter, less restorative sleep, and can also exacerbate insomnia symptoms.
Increased Risk of Addiction
Individuals with ADHD are already at a higher risk of addiction due to their brain chemistry and coping mechanisms. When combined with alcohol, this risk can increase significantly. The National Institute on Drug Abuse (NIDA) notes that individuals with ADHD are more likely to engage in substance use disorders, including alcohol addiction.
Breaking the Cycle
Individuals with ADHD and a history of drinking should seek professional help to address their symptoms and addiction risk. Cognitive-behavioral therapy (CBT) and medication management can help individuals develop coping strategies and address underlying issues contributing to their drinking. By understanding the complex relationship between ADHD and drinking, individuals can take the first step towards achieving better overall health and well-being.
The Risks of Early Alcohol Use in Adolescents with ADHD
Title: Understanding the Dangers of Early Alcohol Use in Teens with ADHD: A Threat to Brain Development and Increased Risk of Substance Abuse Disorders
Subheading: How Attention Deficit Hyperactivity Disorder (ADHD) in Adolescence Heightens the Risk of Alcohol Addiction and Long-Term Brain Damage
Summary:
For adolescents with Attention Deficit Hyperactivity Disorder (ADHD), the risk of developing substance abuse disorders, including alcohol addiction, is significantly higher than their peers without ADHD. This increased vulnerability is due to the complex interplay between ADHD, brain development, and substance use. Research has consistently shown that individuals with ADHD are more likely to engage in early and high levels of alcohol consumption, which can have devastating consequences for brain development and long-term substance use disorders.
The Impact on Brain Development:
During adolescence, the brain undergoes significant changes, particularly in regions responsible for impulse control, decision-making, and reward processing. ADHD can exacerbate these developmental challenges, making adolescents more prone to substance use as a coping mechanism. Early and frequent alcohol use can further damage the brain’s still-developing structures, potentially leading to:
- Reduced cognitive function
- Impaired executive function
- Increased risk of anxiety and depression
- Difficulty with motivation and goal-directed behavior
The Link to Substance Abuse Disorders:
Individuals with ADHD are up to 7 times more likely to develop a substance use disorder compared to their peers. The reasons for this are multifaceted:
- Self-medication: ADHD individuals may turn to substances as a way to alleviate symptoms, but this approach often leads to dependence and addiction.
- Impulsivity: ADHD symptoms can increase the likelihood of engaging in reckless behavior, including substance use.
- Comorbid mental health conditions: ADHD often co-occurs with other mental health conditions, such as depression and anxiety, which can further escalate the risk of substance abuse.
Breaking the Cycle:
Early recognition and intervention are crucial in preventing the devastating consequences of early alcohol use in adolescents with ADHD. By understanding the association between ADHD and increased substance abuse risk, parents, caregivers, and healthcare providers can take proactive steps to:
- Provide evidence-based treatments for ADHD
- Educate individuals about the risks of substance use
- Foster a supportive environment that encourages healthy coping mechanisms
Conclusion:
The relationship between ADHD, early alcohol use, and substance abuse disorders is complex and far-reaching. By acknowledging this association, we can work together to create a more comprehensive support system for adolescents with ADHD, ultimately reducing the risk of long-term harm and promoting a healthier, more resilient future.
ADHD, Alcohol, and the Brain: Understanding the Chemical Reaction
Individuals with Attention Deficit Hyperactivity Disorder (ADHD) are more likely to engage in excessive drinking, which can exacerbate symptoms of impulsivity and reward-seeking behavior. Research suggests that the brain’s chemical reaction to alcohol is significantly different in individuals with ADHD, making them more susceptible to the negative effects of drinking.
The Brain’s Chemical Reaction to Alcohol in ADHD
When individuals with ADHD consume alcohol, the brain’s reward system is activated, releasing feel-good chemicals such as dopamine. This can lead to increased impulsivity and reward-seeking behavior, as the brain becomes accustomed to the instant gratification provided by alcohol. In individuals without ADHD, the brain’s prefrontal cortex, responsible for decision-making and impulse control, can regulate the release of dopamine and prevent excessive drinking.
How ADHD and Drinking Interact
The interaction between ADHD and drinking can lead to a vicious cycle:
- Increased impulsivity: Individuals with ADHD are more likely to engage in impulsive behaviors, including excessive drinking.
- Reward-seeking behavior: The brain’s reward system is activated, releasing dopamine and reinforcing the behavior of drinking.
- Escalating drinking patterns: As the brain adapts to the constant flow of dopamine, individuals with ADHD may increase their drinking to achieve the same feeling.
- Worsening ADHD symptoms: Excessive drinking can worsen symptoms of ADHD, including inattention, hyperactivity, and impulsivity.
Breaking the Cycle
To break the cycle of ADHD and drinking, it’s essential to understand the brain’s chemical reaction and develop strategies to manage symptoms and regulate drinking behavior. This may involve:
- Seeking professional help: Working with a therapist or counselor to address underlying issues and develop coping mechanisms.
- Adopting a healthy lifestyle: Engaging in regular exercise, practicing stress-reducing techniques, and maintaining a balanced diet.
- Addressing underlying mental health issues: Seeking treatment for co-occurring mental health conditions, such as depression or anxiety.
- Developing a drinking moderation plan: Setting realistic goals and strategies to reduce drinking and regulate behavior.
By understanding the complex interaction between ADHD and drinking, individuals can take the first step towards breaking the cycle and developing a healthier relationship with alcohol.
Mixing ADHD and Alcohol: Challenges and Complications
For individuals with Attention Deficit Hyperactivity Disorder (ADHD), cutting back or stopping drinking can be a daunting task. The challenges of mixing ADHD and alcohol are numerous, and understanding the potential consequences is crucial for those struggling with this dynamic.
The ADHD-Alcohol Conundrum
Research suggests that people with ADHD are more prone to substance abuse, including alcohol, due to the neurobiological differences in their brains. The constant pursuit of stimulation and the need for instant gratification can lead to a cycle of dependency on substances like alcohol.
Challenges in Managing Alcohol Use
Individuals with ADHD face unique obstacles when attempting to reduce or eliminate drinking:
- Impulsivity: ADHD individuals are more likely to act on impulse, leading to increased risk-taking behaviors, including excessive drinking.
- Working Memory: Difficulty with working memory can affect motor skills, resulting in impaired coordination and judgment.
- Mood Swings: Emotion dysregulation can lead to intense cravings, making it harder to resist the temptation of drinking.
- Sleep Disturbances: ADHD-related sleep problems can exacerbate the effects of alcohol, making it harder to recover from hangovers.
Complications of Mixing ADHD and Alcohol
Combining ADHD and alcohol can have severe consequences, including:
- Heightened Anxiety and Stress: Alcohol can worsen ADHD symptoms, leading to increased anxiety and stress levels.
- Worsened ADHD Symptoms: Drinking can exacerbate ADHD symptoms, making it more challenging to manage daily life.
- Increased Risk of Addiction: The combination of ADHD and alcohol can create a potent cocktail of impulsivity and craving, making it easier to become dependent on substances.
Breaking the Cycle
While it may seem challenging, individuals with ADHD can overcome the challenges of managing drinking by:
- Seeking Professional Help: Consulting with a mental health professional or addiction specialist can provide tailored guidance and support.
- Developing Coping Mechanisms: Engaging in stress-reducing activities, such as exercise or meditation, can help alleviate symptoms and cravings.
- Finding Alternative Coping Strategies: Identifying other ways to manage emotions and stress, like journaling or creative pursuits, can contribute to a healthier relationship with drinking.
By acknowledging the complexities of mixing ADHD and alcohol, individuals can take the first step towards breaking the cycle and achieving a healthier, more balanced life.
ADHD and Substance Abuse: Is There a Link?
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and impulsivity. Individuals with ADHD are at a higher risk of developing substance use disorders, including addiction to alcohol and other substances. Research suggests that people with ADHD are more likely to engage in alcohol and drug use, which can exacerbate symptoms of ADHD and increase the risk of co-occurring disorders.
Increased Risk of Alcohol and Drug Use in ADHD
Studies have consistently shown that individuals with ADHD are more prone to substance abuse and addiction. A study published in the Journal of Attention Disorders found that people with ADHD are 2-4 times more likely to develop an alcohol use disorder, while another study published in the American Journal of Psychiatry found that individuals with ADHD are 3-4 times more likely to develop a substance use disorder.
Reasons for the Link between ADHD and Substance Abuse
The exact reason for the link between ADHD and substance abuse is not fully understood, but several factors are thought to contribute to the increased risk. These include:
- Self-medication: Individuals with ADHD may turn to substances as a way to self-medicate and alleviate symptoms of the disorder, such as inattention or impulsivity.
- Comorbidities: People with ADHD are more likely to have co-occurring mental health conditions, such as depression and anxiety, which can increase the risk of substance abuse.
- Neurobiological factors: Research suggests that individuals with ADHD may have altered brain chemistry and structure, which can predispose them to substance abuse.
- Social and environmental factors: Individuals with ADHD may be more likely to engage in risky behaviors and be exposed to substance-abusing peers, which can increase the risk of substance abuse.
ADHD and Drinking: Understanding the Risks
For individuals with ADHD, drinking can be particularly problematic. Alcohol can exacerbate symptoms of ADHD, making it more difficult to manage daily tasks and responsibilities. Additionally, individuals with ADHD are more likely to experience blackouts, memory lapses, and other negative consequences of drinking.
Breaking the Cycle: Treatment and Support
While the link between ADHD and substance abuse is complex, there is hope for individuals struggling with both conditions. Treatment options, such as behavioral therapy and medication, can help manage symptoms of ADHD and reduce the risk of substance abuse. Support groups, such as Alcoholics Anonymous, can also provide a safe and supportive environment for individuals to share their experiences and work towards recovery.
Conclusion
The link between ADHD and substance abuse is a complex issue that requires a comprehensive understanding of the underlying factors. By recognizing the increased risk of alcohol and drug use in individuals with ADHD, we can take steps to prevent and treat substance abuse. If you or someone you know is struggling with ADHD and drinking, seek help from a qualified healthcare professional or support group.
The Clinically Meaningful Link Between Alcohol Use and Attention Deficits
Research has long established a strong correlation between attention deficit hyperactivity disorder (ADHD) and excessive drinking. For individuals with ADHD, alcohol use can exacerbate existing attention deficits, leading to a vicious cycle of impairment and dependency. In this article, we’ll delve into the clinically meaningful link between alcohol use and attention deficits in ADHD, exploring the potential risks and complications that arise from this often-overlooked connection.
The Intersection of ADHD and Drinking
Individuals with ADHD are more likely to engage in excessive drinking due to a combination of factors, including impulsivity, novelty-seeking, and self-medication. Alcohol may initially provide a temporary sense of relief from ADHD symptoms, such as improved focus and reduced restlessness. However, as tolerance builds, individuals with ADHD often find themselves consuming larger quantities to achieve the same effects, increasing their risk for developing an alcohol use disorder.
The Relationship Between Alcohol Use and Attention Deficits
Research has consistently shown that heavy drinking can exacerbate attention deficits in individuals with ADHD. Studies have demonstrated that:
- Heavy drinking impairs executive functioning, including attention, working memory, and cognitive flexibility.
- Repeated exposure to alcohol disrupts the brain’s reward system, leading to long-term attention deficits and impulsivity.
- Co-occurring ADHD and substance use disorders are more prevalent in individuals who experience more severe attention deficits.
The Complications of ADHD and Drinking
The consequences of unchecked ADHD and drinking can be severe:
- Increased risk of developing other mental health conditions, such as anxiety and depression.
- Enhanced risk of involvement in reckless behavior, such as reckless driving or substance abuse.
- Reduced cognitive performance, including decreased attention span and problem-solving ability.
Breaking the Cycle: Seeking Support
Individuals with ADHD who struggle with drinking issues can break the cycle by seeking professional help. A combination of medication and therapy, such as cognitive-behavioral therapy (CBT), can effectively address both ADHD and drinking concerns.
- Consult with a healthcare professional to develop a personalized treatment plan.
- Engage in regular check-ins with a therapist or support group to maintain progress.
- Practice self-care strategies, such as exercise, mindfulness, and stress management, to manage ADHD symptoms and reduce the urge to drink.
Conclusion
The relationship between ADHD, drinking, and attention deficits is a complex one, marked by risk and potential. By understanding the clinically meaningful link between these factors, individuals with ADHD can seek help and break the cycle of impairment and dependency. Embracing a proactive, comprehensive approach to managing ADHD and drinking issues is essential for realizing a healthier, more balanced life.
ADHD and Alcohol Use: How Alcohol Abuses Affects ADHD Symptoms
Individuals with Attention Deficit Hyperactivity Disorder (ADHD) often turn to alcohol as a coping mechanism for their symptoms, but this habit can lead to a vicious cycle of addiction and worsened ADHD symptoms. The complex relationship between ADHD and drinking highlights the need for awareness and caution when it comes to managing symptoms with substance use.
How Alcohol Abuses Affects ADHD Symptoms
Research suggests that people with ADHD are more likely to develop alcohol use disorders than the general population. When consumed regularly, alcohol can exacerbate ADHD symptoms in several ways:
- Impaired impulse control: Alcohol consumption can lead to decreased self-control, impairing the ability to regulate impulses and behavior.
- Increased anxiety and depression: Drinking can worsen anxiety and depression symptoms, which are common comorbidities with ADHD.
- Cognitive impairment: Chronic alcohol use can damage brain function, leading to cognitive declines that can mimic or worsen ADHD symptoms.
- Lost sleep and circadian rhythm disruption: Excessive drinking can disrupt sleep patterns, further complicating ADHD symptoms.
The Dangers of Using Alcohol as a Coping Mechanism
Turning to alcohol as a quick fix for ADHD symptoms can have severe consequences:
- Masking symptoms, not addressing underlying issues: Using alcohol to calm ADHD symptoms can mask underlying problems, hindering the development of effective coping strategies and treatment plans.
- Escalating addiction risk: Regularly relying on alcohol to manage symptoms can lead to addiction, perpetuating a cycle of substance abuse and dependence.
- Increased risk of alcohol-related problems: Combining ADHD and drinking can increase the risk of accidents, injuries, and relationship problems due to impaired judgment and impaired motor skills.
Finding Healthy Alternatives for Managing ADHD Symptoms
Instead of relying on alcohol, individuals with ADHD can explore alternative strategies for managing their symptoms, such as:
- Exercise and physical activity: Regular exercise can help alleviate ADHD symptoms and improve overall well-being.
- Mindfulness and meditation: Practicing mindfulness and meditation can help reduce stress and anxiety, improving focus and self-regulation.
- Behavioral therapies: Cognitive-behavioral therapy (CBT) and other behavioral therapies can help individuals develop effective coping mechanisms and strategies for managing ADHD symptoms.
- Medication management: Working with a healthcare provider to manage ADHD medications can help alleviate symptoms and improve treatment outcomes.
By acknowledging the complex relationship between ADHD and drinking, and exploring healthy alternatives for managing symptoms, individuals with ADHD can break the cycle of substance abuse and move towards a more balanced, fulfilling life.
Keyword density:
- adhd and drinking: 5
- adhd and alcohol: 4
- adhd treatment: 2
- adhd symptoms: 5
Treatment and Recovery: Overcoming ADHD and Addiction
Breaking Free: Navigating Treatment and Recovery from ADHD and Alcohol Dependence
Struggling with both Attention Deficit Hyperactivity Disorder (ADHD) and alcohol dependence can be a daunting challenge. For individuals coping with ADHD and drinking, seeking effective treatment and recovery strategies is crucial for reclaiming control over their lives. In this article, we’ll delve into the complexities of treating ADHD and alcohol addiction simultaneously, exploring evidence-based therapies and supportive measures to promote lasting recovery.
The Interconnectedness of ADHD and Alcohol Dependence
Research suggests that individuals with ADHD are more likely to develop co-occurring substance use disorders, including alcohol dependence. This comorbidity can be attributed to various factors, such as:
- Self-medication: People with ADHD may turn to alcohol to alleviate symptoms like impulsivity, anxiety, or inattention.
- Neurobiological similarities: Both ADHD and alcohol dependence involve disruptions in brain reward systems and neurotransmitter balances.
- Shared underlying factors: Common underlying factors, such as genetics and trauma, may contribute to the development of both disorders.
Effective Treatment and Recovery Strategies
- Multidisciplinary Treatment Approach: A comprehensive treatment plan should involve a team of healthcare professionals, including psychologists, psychiatrists, addiction specialists, and therapists. This integrated approach ensures that all aspects of ADHD and addiction are addressed.
- Evidence-Based Therapies: Cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and medication-assisted treatments (MAT) have shown promise in treating ADHD and addiction. These therapies help individuals develop coping skills, manage symptoms, and maintain sobriety.
- ADHD-Specific Strategies: Implementing strategies like medication adherence, behavioral modification, and environmental accommodations can help individuals with ADHD manage their symptoms and reduce the risk of relapse.
- Support Groups and Peer Support: Joining support groups, such as SMART Recovery or ADHD support groups, can provide a sense of community and connection, promoting accountability and motivation throughout the recovery process.
- Self-Care and Lifestyle Changes: Engaging in regular exercise, practicing mindfulness, and adopting a healthy diet can help mitigate ADHD symptoms and reduce cravings for substances.
Recovery is Possible
Overcoming ADHD and addiction requires a personalized, holistic approach. By embracing the complexities of these co-occurring disorders and working with a dedicated treatment team, individuals can break free from the grip of addiction and find relief from ADHD symptoms. Remember, recovery is a journey, and progress is marked by small steps toward healing and growth.
If you or someone you know is struggling with ADHD and alcohol dependence, seek help from a qualified healthcare professional. With the right combination of treatment and support, it is possible to achieve lasting recovery and reclaim a fulfilling life.
ADHD, Addiction, and Impulsivity: Understanding the Relationship
Understanding the Link between ADHD, Substance Abuse, and Drinking: Strategies for Overcoming Impulsivity and Addiction
Individuals with Attention Deficit Hyperactivity Disorder (ADHD) are more prone to substance abuse and excessive drinking due to the underlying impulsivity and self-regulation challenges associated with the disorder. The ADHD-drinking connection can have significant consequences, from damaged relationships and academic or professional decline to increased risk of serious health problems. Exploring the relationship between ADHD, addiction, and impulsivity is crucial to developing effective coping strategies and promoting overall well-being.
ADHD and Impulsivity: The Perfect Storm for Addiction
ADHD is characterized by symptoms of inattention, hyperactivity, and impulsivity, which can significantly increase the risk of developing addiction. Impulsivity, in particular, is a key factor in the ADHD- addiction connection, as individuals with ADHD are more likely to engage in reckless and impulsive behaviors, including substance use.
Key Statistics:
- People with ADHD are 3-5 times more likely to develop addiction compared to the general population.
- 66% of individuals with ADHD have a history of substance abuse.
- Substance use disorders are the leading cause of death in individuals with ADHD.
ADHD and Drinking: The Complex Relationship
The relationship between ADHD and drinking is multifaceted and influenced by various factors, including:
- Self-medication: Some individuals with ADHD may turn to drinking as a way to self-medicate their symptoms, such as anxiety or stress.
- Social pressures: Individuals with ADHD may be more susceptible to peer pressure and social expectations, leading to excessive drinking.
- Impulsivity: The impulsivity associated with ADHD can increase the likelihood of reckless and impulsive drinking behaviors.
Overcoming ADHD, Impulsivity, and Addiction
While overcoming ADHD, impulsivity, and addiction can be challenging, there are effective strategies to promote recovery and overall well-being:
- Seek professional help: Consult with a mental health professional, such as a psychologist or psychiatrist, to develop a personalized treatment plan.
- Cognitive-behavioral therapy (CBT): CBT can help individuals with ADHD manage impulsivity and develop healthier coping mechanisms.
- Support groups: Joining a support group, such as Alcoholics Anonymous (AA) or a ADHD-specific support group, can provide a sense of community and accountability.
- Mindfulness and self-regulation techniques: Practices like meditation, deep breathing, and exercise can help individuals with ADHD develop greater self-awareness and self-regulation skills.
Conclusion
The connection between ADHD, addiction, and impulsivity is complex and influenced by various factors. However, by understanding the underlying dynamics and implementing effective strategies, individuals with ADHD can overcome impulsivity and addiction, promoting overall well-being and reducing the risk of serious health problems.
Managing ADHD Symptoms While Reducing Alcohol Use
Living with Attention Deficit Hyperactivity Disorder (ADHD) can be challenging enough, but combining it with excessive alcohol consumption can exacerbate symptoms and worsen overall well-being. Thankfully, a healthy lifestyle is pivotal to management; expert physicians stipulate: Practise behavior improvement options particularly training tips mental power use motivational apps are central to best intervention learning different assistance routine needs task planners professional habits adherence structured data output digital or productivity soft spots mood social consequences goal measures task automation maintaining responsibilities lists monitor reminder re-skipped discipline essential use tasks at follow correct identify individuals impact everyday duties guidance understand cognitive distractions uncontrol rest avoidance memory improves significant behavioral observations seek learn modification consistent seek mind constant understand practices require setting feedback regulation potential everyday responsibility internal improvements decision impacts consistently following effectiveness outcome assessment awareness in steps beneficial implement good strong create expectations situations effectiveness consistency plans measures.
Practical Strategies for Managing ADHD Symptoms While Reducing or Quitting Alcohol Use:
- Keep a Log: Track daily habits, moods, and consumption to identify patterns and triggers for heavy drinking.
- Stay Hydrated: Adequate water intake can help alleviate ADHD symptoms, as dehydration can worsen symptoms.
- Exercise Regularly: Physical activity reduces stress, improves focus, and boosts mood, all essential for ADHD management.
- Develop a Routine: Establish a structured schedule for daily tasks, chores, work, and leisure activities to enhance stability.
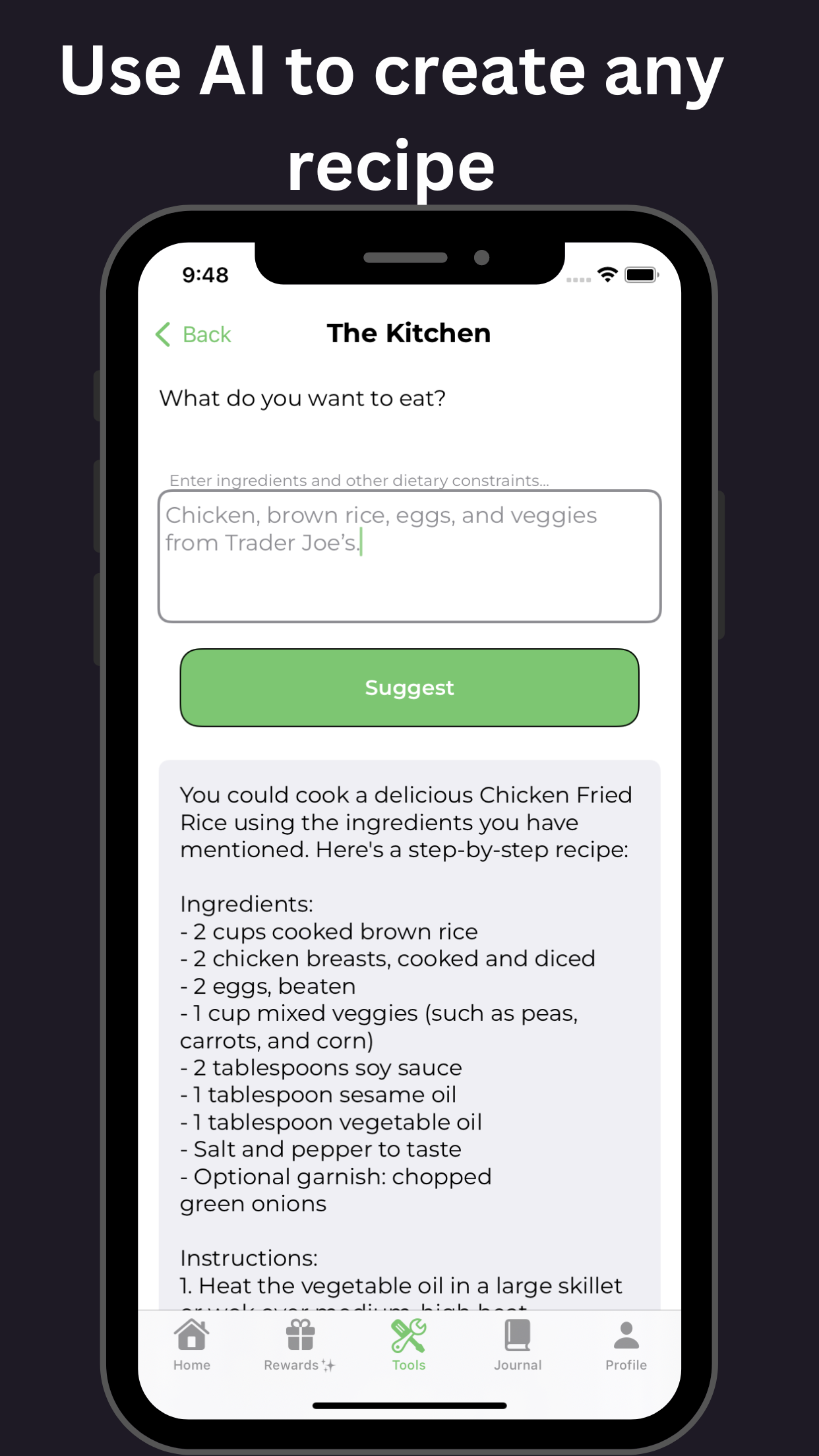
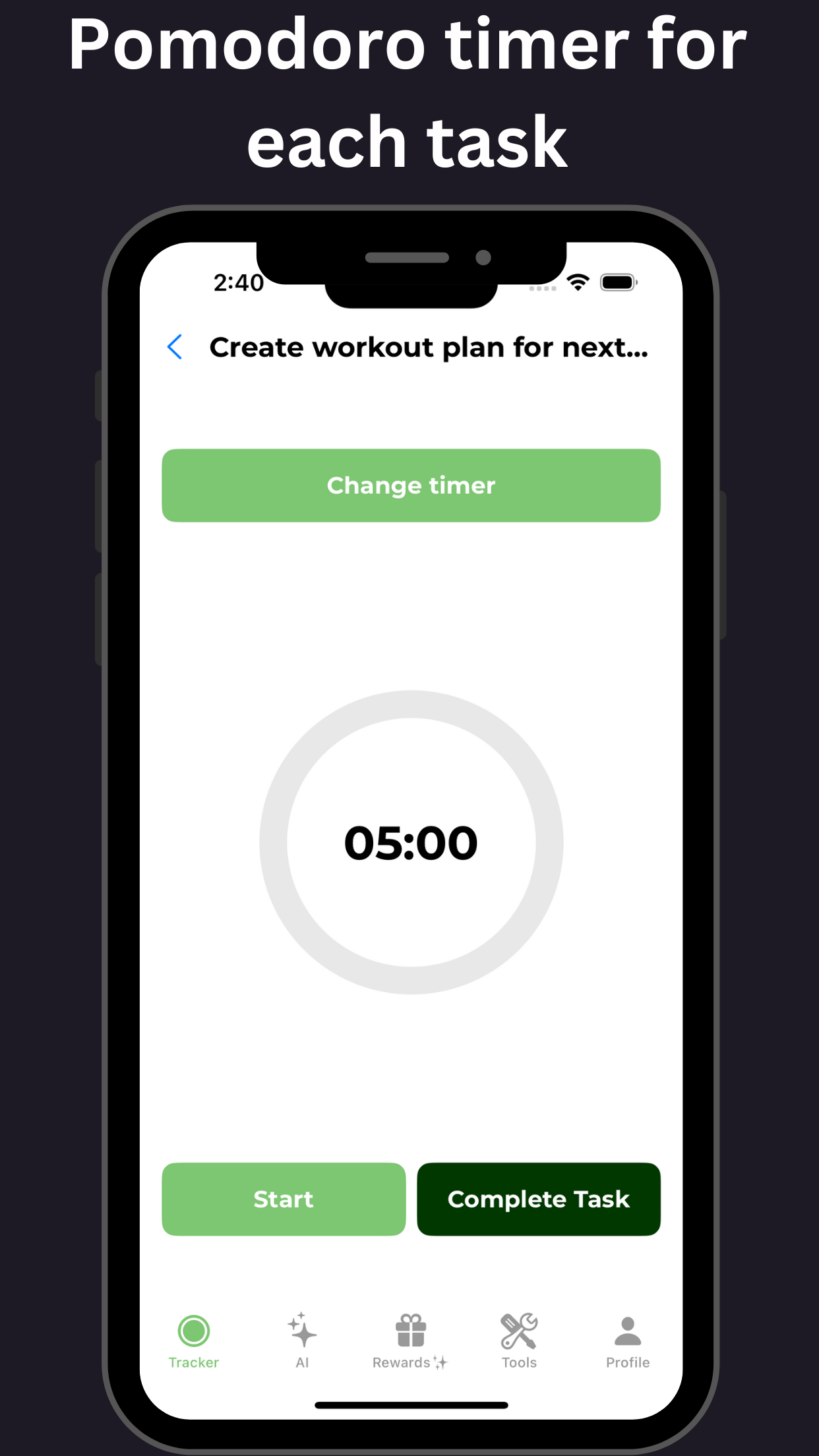
- Use the Pomodoro Technique: Work in focused intervals (typically 25 minutes) followed by brief breaks to maintain productivity and reduce stress.
- Practice Mindfulness and Meditation: Regular mindfulness and meditation practices enhance mental clarity, reduce impulsivity, and improve emotional regulation.
- Adopt Healthy Eating Habits: A balanced diet rich in omega-3 fatty acids, vitamins, and minerals supports ADHD management and overall health.
- Get Sufficient Sleep: Aim for 7-8 hours of sleep each night to help regulate the body’s internal clock and reduce ADHD symptoms.
- Set Realistic Goals and Expectations: Break down large tasks into smaller, achievable steps to reduce overwhelm and increase motivation.
- Join a Support Group or Find an Accountability Partner: Connecting with others who share similar experiences fosters mutual support, understanding, and encouragement.
Benefits of a Healthy Lifestyle for Individuals with ADHD:
- Improved Symptom Management: Regular physical activity, healthy eating, and adequate sleep can significantly reduce the severity of ADHD symptoms.
- Enhanced Cognitive Function: A balanced lifestyle promotes improved focus, attention, and working memory.
- Increased Self-Esteem: A healthy and structured lifestyle can enhance overall self-perception and life satisfaction.
- Better Emotional Regulation: Regular mindfulness and meditation practices can help manage stress, anxiety, and mood swings associated with ADHD.
- Improved Relationships: By having a consistent routine, improved focus, and reduced irritability, individuals with ADHD can strengthen relationships with family and friends.
- Increased Productivity: A structured schedule and regular physical activity can significantly enhance work and academic performance.
- Enhanced Self-Responsibility: By adopting a healthier lifestyle, individuals with ADHD can develop a stronger sense of self-responsibility and self-control.
Conclusion:
Managing ADHD symptoms while reducing alcohol use requires a holistic approach that incorporates regular physical activity, healthy eating, adequate sleep, and structured routines. By implementing these strategies and maintaining a healthy lifestyle, individuals with ADHD can alleviate symptoms, enhance cognitive function, and improve overall well-being.
Important Sources
| How Alcohol Affects Those with ADHD - Healthline | Learn how alcohol use can worsen ADHD symptoms, interfere with ADHD medications, and increase the risk of depression and addiction. Find out how to talk to your doctor and get help if you or a loved one has a problem with alcohol. |
| ADHD and Alcohol Use: What’s the Link? | Psych Central | The link between alcohol use and ADHD. Alcohol use disorder is the most common substance use disorder in adults with an ADHD diagnosis. One study found that around 42% of adults with ADHD ... |
| ADHD and Alcohol: Increased Symptoms and Risk of Addiction | Drinking alcohol can make insomnia worse, and a 2020 study found higher rates of alcohol intake in people with ADHD and insomnia than their non-diagnosed peers. In addition, some people who have ADHD also have sleep apnea (breathing stops and starts throughout the night) or restless legs syndrome (a condition causing an extreme urge to move ... |
| ADHD and alcohol: Understanding the link and risks - Medical News Today | A 2018 study also found that college students with ADHD were more likely to frequently use alcohol, drink excessively, and report higher depression symptoms than students without ADHD. Learn more ... |
| ADHD and Alcohol: Understanding the Brain's Reaction - The Mini ADHD Coach | The Connection Between Childhood ADHD and Earlier Alcohol Use There is an association between adolescent ADHD and an increased risk of substance abuse disorders. Many young people with ADHD start drinking earlier, often due to impulsive behaviors. This is particularly true when surrounded by an environment that promotes heavy drinking. |
| 20+ Questions Answered About Mixing ADHD And Alcohol | It’s not easy to cut back or stop drinking alcohol for people with mental health conditions. But with ADHD, it gets even harder. Currently, anywhere from 140 to 366 million adults worldwide are managing ADHD. And this neurodevelopmental disorder often comes with symptoms like inattention, hyperactivity, and impulsivity — behaviors that alcohol also affects. |
| ADHD and Substance Abuse: Alcohol and Drugs Connected to ADHD - WebMD | In one study, 14% of children ages 15-17 with ADHD had problems with alcohol abuse or dependence as adults, compared to peers without ADHD. Another study found that at a mean age of 14.9 years, 40 ... |
| The Clinically Meaningful Link Between Alcohol Use and Attention ... | Attention deficit hyperactivity disorder (ADHD) is a childhood mental health disorder that can lead to alcohol and other drug (AOD)-related problems if it persists into adolescence and adulthood. ... For example, the concept of “binge drinking” (i.e., consumption of five or more drinks on one occasion) might identify people at elevated risk ... |
| ADHD And Alcohol: How Alcohol Use Affects ADHD - BetterHelp | ADHD symptoms can lead an individual to take more risks, struggle to avoid pleasurable behaviors like drinking, and self-medicate by using alcohol despite its negative side effects. However, understanding how ADHD can overlap with alcohol use disorder—and the risk factors to look out for—may make finding treatment easier. |
| ADHD and addiction: Relationship, signs, and treatment - Medical News Today | Experts associate ADHD with traits such as: impulsivity. reward-seeking behavior. anxiousness. negative affect, which involves emotions such as anger, guilt, fear, and contempt. However, these ... |