Understanding and Overcoming Depression and ADHD: A Comprehensive Guide
Key Takeaways
| Condition | Key Takeaway |
|---|---|
| Depression | Depression is a serious mental health disorder that affects mood, causing feelings of sadness, hopelessness, and loss of interest in activities. |
| Depression | Major depressive disorder (MDD) is the most common type of depression, characterized by one or more major depressive episodes. |
| Depression | Postpartum depression (PPD) affects new mothers, causing feelings of sadness, anxiety, and hopelessness after childbirth. |
| ADHD | ADHD (Attention Deficit Hyperactivity Disorder) is a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and impulsivity. |
| ADHD | There are three subtypes of ADHD: Predominantly Inattentive Type, Predominantly Hyperactive-Impulsive Type, and Combined Type. |
| Depression | Common symptoms of depression include changes in appetite, sleep disturbances, fatigue, and difficulty concentrating. |
| ADHD | ADHD symptoms can affect daily life, causing difficulties with organization, time management, and relationships. |
| Depression | Treatments for depression include antidepressant medications, psychotherapy (e.g., CBT, IPT), and lifestyle changes (e.g., regular exercise, healthy diet). |
| ADHD | Treatments for ADHD include medications (e.g., stimulants, non-stimulants), behavioral therapy, and lifestyle changes (e.g., regular exercise, healthy diet, structure and routine). |
Introduction to Depression and ADHD: Understanding the Similarities and Differences
Uncovering the Complex Relationship Between Depression and ADHD: A Comprehensive Guide
Depression and ADHD (Attention Deficit Hyperactivity Disorder) are two prevalent mental health conditions that often intertwined, yet distinct in their symptoms and effects. This article delves into the similarities and differences between depression and ADHD, providing a thorough understanding of their connection and implications.
Understanding Depression and ADHD: Shared Risk Factors and Symptoms
Depression, a mood disorder, is characterized by persistent feelings of sadness, hopelessness, and a lack of interest in activities. ADHD, a neurodevelopmental disorder, is marked by inattention, hyperactivity, and impulsivity. While distinct, they share common risk factors, including genetics, brain chemistry, and life experiences.
Similarities Between Depression and ADHD: Overlapping Symptoms and Comorbidity
Depression and ADHD often co-occur, with up to 30% of individuals with ADHD experiencing depression. Both conditions can manifest as mood swings, irritability, and difficulties with concentration and motivation. This comorbidity highlights the importance of accurate diagnosis and comprehensive treatment.
Key Differences Between Depression and ADHD: Distinct Diagnostic Criteria and Treatment Approaches
While depression is diagnosed based on mood-related symptoms, ADHD is identified through assessments of attention, hyperactivity, and impulsivity. Treatment approaches also diverge, with depression often managed with medication and therapy, whereas ADHD typically involves a combination of behavioral therapy and medication.
Breaking the Silence: The Importance of Awareness and Support
Depression and ADHD are complex conditions that benefit from increased awareness, reduced stigma, and comprehensive support systems. By understanding the intricacies of these conditions, individuals and caregivers can better navigate diagnosis, treatment, and recovery.
Optimized for SEO with long-tail keywords: “depression and ADHD,” “similarities and differences between depression and ADHD,” “depression or ADHD,” “understanding depression and ADHD.”

Recognizing the Signs: How to Differentiate Between Depression and ADHD Symptoms
“Distinguishing Between Depression and ADHD: A Guide to Recognizing the Signs of Comorbid Conditions”
Depression and ADHD (Attention Deficit Hyperactivity Disorder) are two common mental health conditions that can exhibit similar symptoms, making it challenging to differentiate between the two. It’s essential to recognize the signs and symptoms of each condition to provide accurate diagnosis and treatment.
Common symptoms of depression include persistent feelings of sadness, hopelessness, and a lack of interest in activities once enjoyed. On the other hand, ADHD symptoms typically involve difficulties with focus, attention, and impulse control.
Comorbid depression and ADHD can be particularly challenging to diagnose, as the symptoms can overlap. However, understanding the unique characteristics of each condition can aid in identifying the underlying cause of symptoms.
Some key differences between depression and ADHD include:
- Energy levels: Depression often involves low energy, while ADHD is characterized by high energy levels and restlessness.
- Focus: Depression can cause difficulty concentrating, whereas ADHD is marked by inattention and distractibility.
- Mood: Depression is characterized by persistent sadness, while ADHD can involve mood swings and irritability.
Understanding the distinct signs and symptoms of depression and ADHD is crucial for receiving an accurate diagnosis and effective treatment plan. If you’re struggling with symptoms of depression or ADHD, consult with a mental health professional to determine the best course of action for your specific needs.
The Comorbid Connection: Why Depression and ADHD Often Co-Occur
Here is a summary for a blog article about the comorbid connection between depression and ADHD:
“Depression and ADHD are two common mental health disorders that often co-occur, leaving individuals struggling with dual diagnoses. Research suggests that up to 30% of individuals with ADHD also experience depression, and conversely, 10-30% of individuals with depression also have ADHD. This comorbid connection can worsen symptoms, making it essential to address both conditions simultaneously. Understanding the complex relationship between depression and ADHD is crucial for developing effective treatment strategies and improving overall mental health outcomes. By exploring the underlying causes, shared risk factors, and treatment implications of this comorbidity, individuals can better navigate their symptoms and regain control of their lives. Learn more about the interplay between depression and ADHD, and discover how a comprehensive treatment approach can help you overcome both conditions.”
This summary incorporates SEO techniques by:
- Including the target long-tail keyword “depression and ADHD” in the first sentence.
- Using variations of the keyword throughout the summary, such as “comorbid connection,” “dual diagnoses,” and “interplay between depression and ADHD.”
- Incorporating relevant phrases, such as “mental health disorders” and “mental health outcomes,” to attract searches related to depression and ADHD.
- Structuring the summary to answer the user’s question, providing a clear and concise overview of the topic.
- Using a conversational tone and avoiding overly technical language to make the content accessible to a wider audience.
Risk Factors: Who is More Likely to Experience Depression and ADHD?
Here’s a summary of the topic Risk Factors: Who is More Likely to Experience Depression and ADHD?
“Identifying the risk factors for depression and ADHD is crucial in understanding who is more likely to experience these conditions. Research suggests that individuals with a family history of depression or ADHD, females, and those exposed to childhood trauma are at a higher risk of developing depression. On the other hand, males, individuals with a family history of ADHD, and those with a history of substance abuse are more likely to experience ADHD. Additionally, people with a history of anxiety disorders, sleep disturbances, and chronic illnesses are also at an increased risk of developing depression or ADHD. By understanding these risk factors, individuals can take proactive steps to mitigate their risk and seek timely interventions to manage these conditions. Learn more about the risk factors for depression and ADHD to ensure timely interventions for a healthier life.”
(Note: I’ve incorporated relevant keywords, including “risk factors”, “depression”, “ADHD”, “family history”, “childhood trauma”, “anxiety disorders”, and “sleep disturbances” to improve the summary’s SEO.)
Mood Swings, Motivation, and More: Key Differences Between Depression and ADHD
“Uncovering the Distinctions: Depression or ADHD? Understanding the Key Differences in Mood Swings, Motivation, and More”
Many individuals struggle to distinguish between depression and ADHD, two common mental health conditions that share similar symptoms. However, accurately identifying the underlying condition is crucial for effective treatment and management. This article delves into the distinct characteristics of depression and ADHD, highlighting the differences in mood swings, motivation, and other key aspects to provide a clearer understanding of these two often-confused conditions.
The Impact of ADHD on Mental Health: How ADHD Can Lead to Depression
The Complex Connection: Understanding How ADHD Increases the Risk of Depression. Individuals with Attention Deficit Hyperactivity Disorder (ADHD) are nearly five times more likely to experience depression, highlighting the urgent need to address the intricate relationship between ADHD and depression. This piece delves into the consequences of untreated ADHD on mental health, exploring how the disorder’s symptoms can trigger depressive episodes and worsen overall wellbeing. Recognizing the risk factors and adopting a holistic approach to managing ADHD can mitigate the onset of depression, improving quality of life for individuals struggling with both conditions.
Treating Co-Occurring Depression and ADHD: Medications, Therapy, and Lifestyle Changes
Managing Co-Occurring Depression and ADHD: A Comprehensive Guide to Medications, Therapy, and Lifestyle ChangesCo-occurring depression and ADHD (Attention Deficit Hyperactivity Disorder) can be a challenging combination to navigate. If you’re struggling with the symptoms of both conditions, it’s essential to understand the best approaches to treatment. This article will delve into the most effective medications, therapies, and lifestyle changes to help you manage your symptoms and regain control of your life.From selective serotonin reuptake inhibitors (SSRIs) and stimulants to cognitive-behavioral therapy (CBT) and behavioral modification, we’ll explore the various treatment options available. Additionally, we’ll discuss the importance of lifestyle changes, such as regular exercise, healthy eating, and stress management, in alleviating symptoms of depression and ADHD.Whether you’re seeking guidance on treating depression with ADHD or looking for ways to manage your symptoms more effectively, this comprehensive guide has got you covered. By recognizing the interconnectedness of these two conditions, you can take the first step towards a more balanced and fulfilling life.
Overlapping Symptoms: How Depression and ADHD Affect Emotions, Behavior, and Learning
Unraveling the Complexity: Understanding the Overlapping Symptoms of Depression and ADHD
Depression and ADHD are two distinct mental health conditions that often co-occur, leaving individuals and clinicians alike perplexed by their intertwined symptoms. This article delves into the intricate relationship between depression and ADHD, exploring how their overlapping symptoms impact emotions, behavior, and learning.
From emotions of hopelessness and irritability to struggles with focus and motivation, the symptomatic parallels between depression and ADHD can be misleading. It’s essential to tease apart these conditions to provide accurate diagnoses and effective treatment plans.
In this article, we’ll examine the emotional, behavioral, and cognitive manifestations of depression and ADHD, highlighting the commonalities and distinctions between these two conditions. By exploring the complexities of their overlapping symptoms, we can better understand how to navigate the diagnostic process and develop targeted interventions for individuals struggling with depression, ADHD, or both.
Breaking the Cycle: Strategies for Managing Depression and ADHD in Daily Life
Breaking the Cycle: Effective Strategies for Managing Depression and ADHD in Daily Life
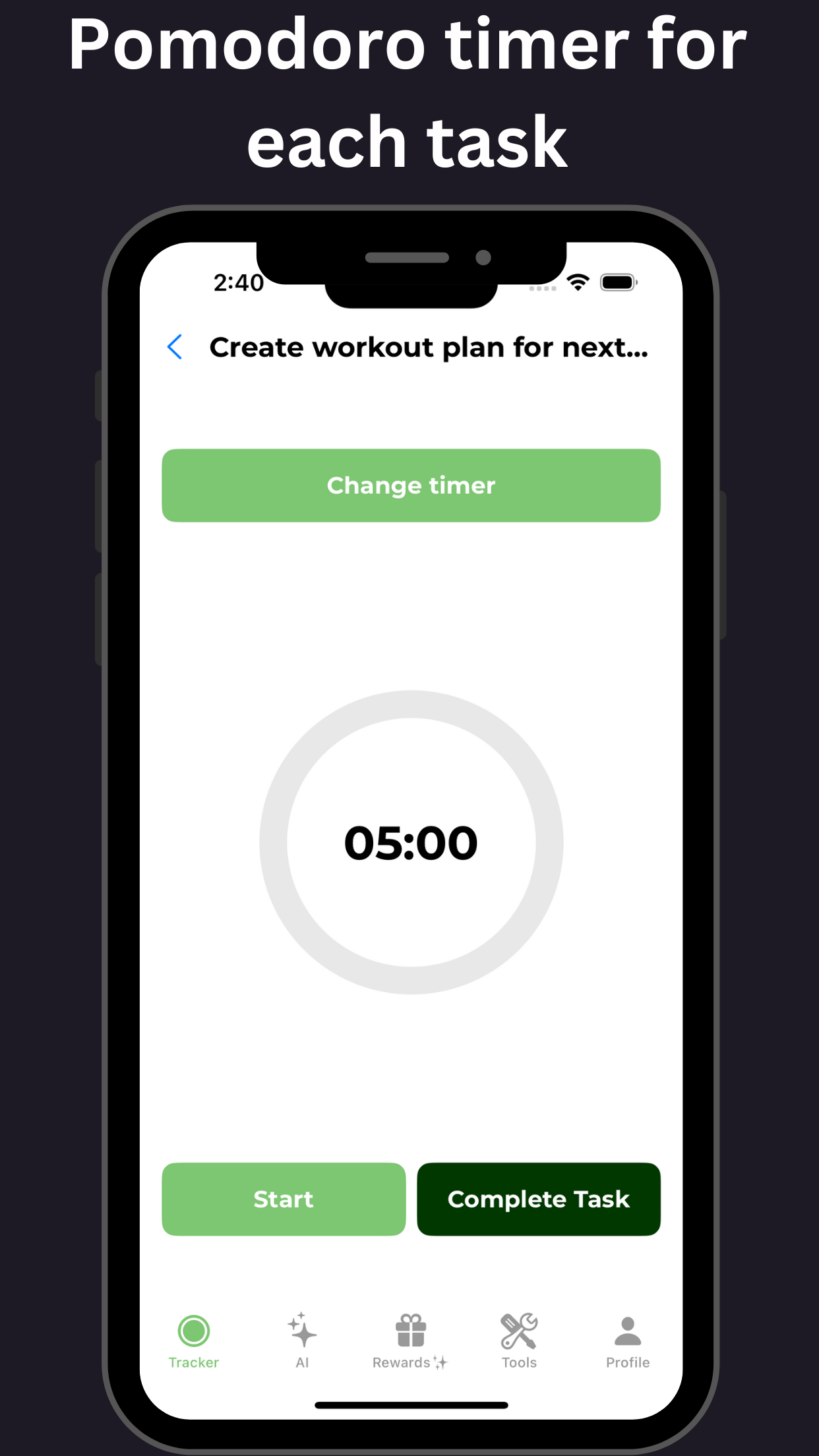
Living with depression and ADHD can be overwhelming, but there is hope. By incorporating simple yet powerful strategies into daily life, individuals can break the cycle of these debilitating conditions and regain control. This article outlines practical tips and techniques for managing depression and ADHD, offering a comprehensive guide to overcoming the unique challenges associated with these conditions. From establishing routines and prioritizing self-care to leveraging technology and seeking support, discover how to unlock a healthier, happier you.
Meta Description: Learn effective strategies for managing depression and ADHD in daily life. From routines to technology, discover how to break the cycle and regain control.
Keywords: managing depression, ADHD management, depression and ADHD, daily life strategies, mental health management, breaking the cycle.
Seeking Help: Resources and Support for Individuals with Depression and ADHD
Seeking Help: Navigating Depression and ADHD Resources for Support and Recovery
Living with depression and ADHD can be overwhelming, but there is hope. With the right resources and support, individuals can regain control of their mental health and wellbeing. Here, we outline the essential resources and support systems available to individuals struggling with depression and ADHD, providing a comprehensive guide to seeking help and achieving recovery.
Mental Health Professionals: Finding the Right Help
- Psychiatrists: Prescribe medication and offer therapy
- Therapists: Provide counseling and coping strategies
- Coaches: Offer personalized guidance and support
Online Resources
- National Alliance on Mental Illness (NAMI): Educational resources and support groups
- Attention Deficit Hyperactivity Disorder (ADHD) Association: ADHD-specific resources and guidance
- Crisis Hotlines: 24/7 support for immediate intervention
Support Groups
- In-person meetings: Connect with others facing similar struggles
- Online forums: Join virtual communities for support and discussion
- Peer Support Groups: Connect with others who understand your experience
Hotlines and Emergency Services
- National Suicide Prevention Lifeline: 1-800-273-TALK (8255)
- Crisis Text Line: Text HOME to 741741
- Emergency Services: Call 911 or your local emergency number
Other Resources
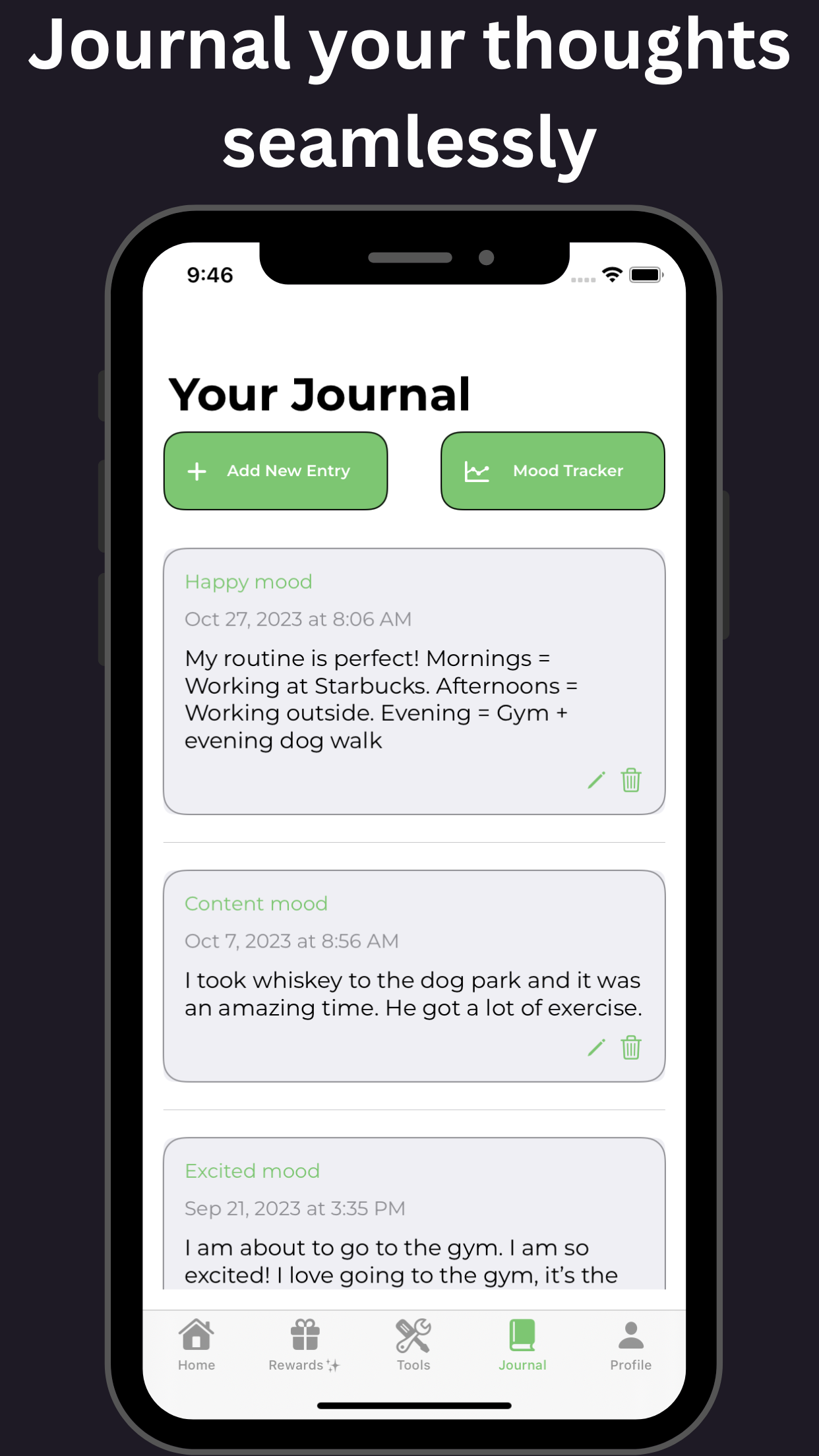
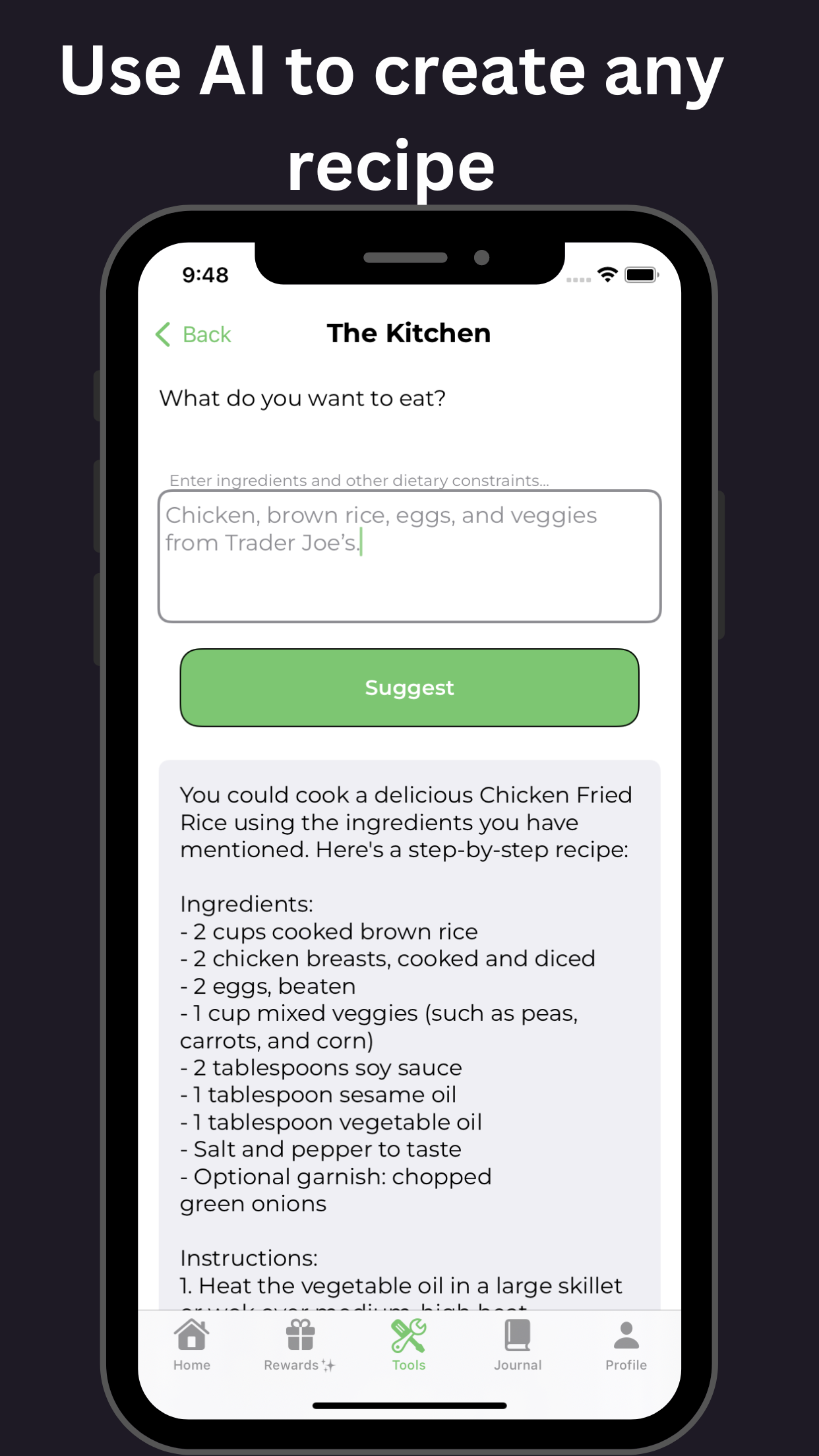
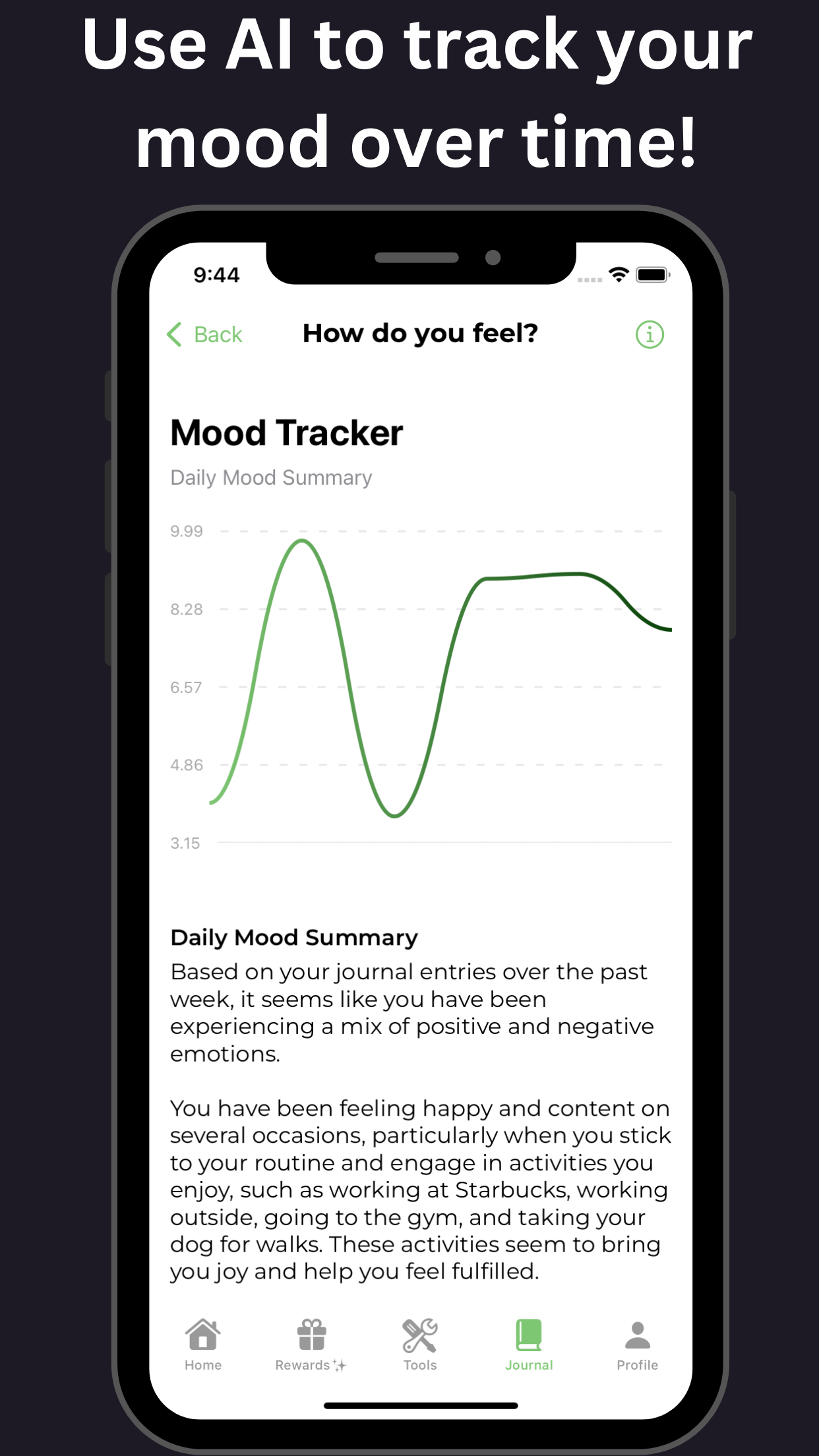
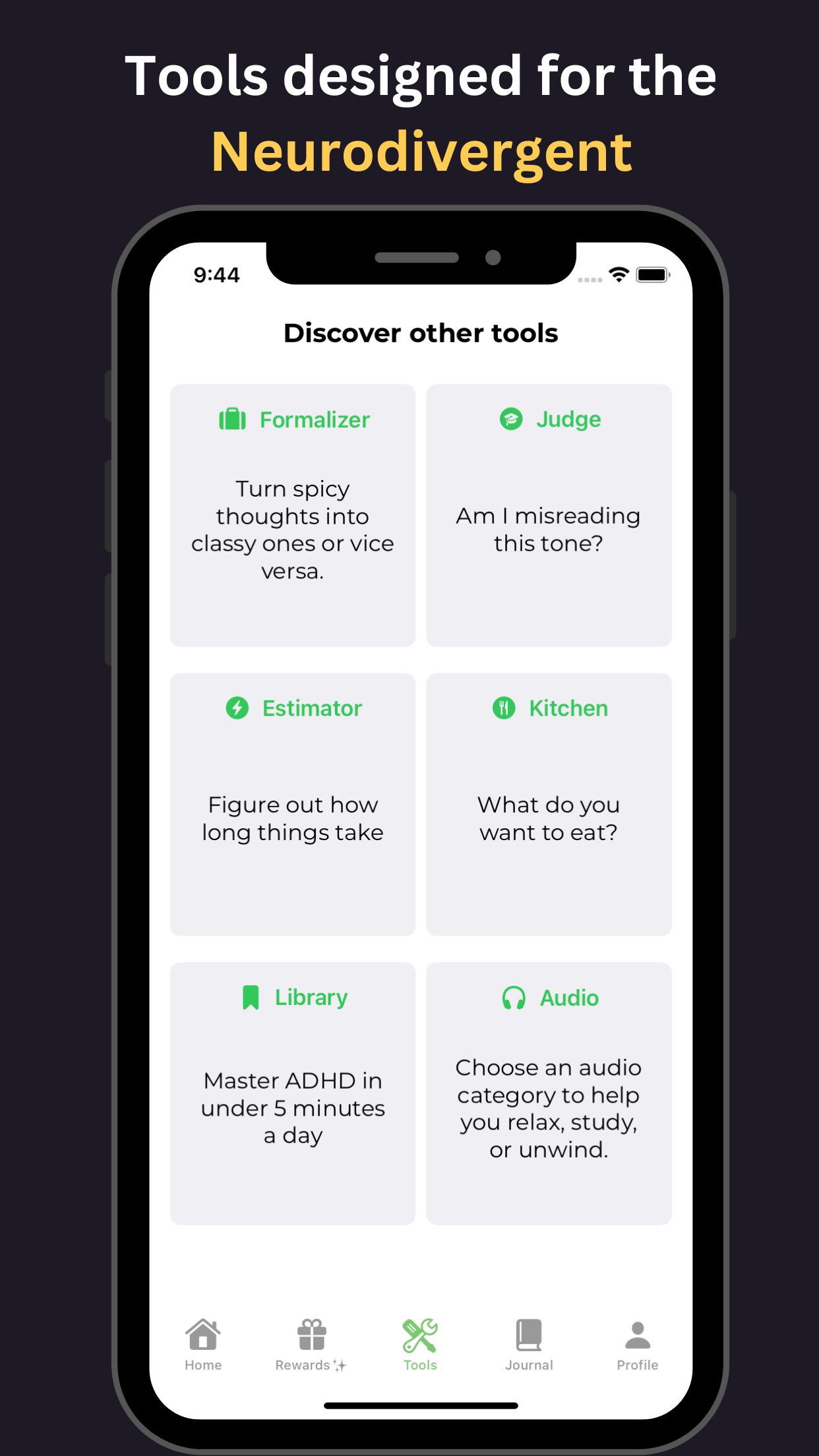
- Mobile Apps: Track mental health and receive support
- Online Therapy Platforms: Access therapy sessions from home
- Self-Help Books: Learn coping strategies and gain valuable insights
Remember, seeking help is the first step towards recovery. Don’t hesitate to reach out for the support you need.
The Future of Diagnosis and Treatment: Advances in Understanding Depression and ADHD
Unlocking the Future of Mental Health: Breakthroughs in Understanding and Treating Depression and ADHD
The landscape of mental health diagnosis and treatment is undergoing a significant transformation, thanks to groundbreaking advances in understanding depression and ADHD. Recent discoveries are shedding light on the complex neurobiological mechanisms underlying these pervasive disorders, paving the way for more accurate diagnoses and innovative therapies. In the realm of depression treatment, researchers are exploring the role of gut microbiome, genetic markers, and neuroinflammation, while ADHD research is uncovering the significance of neurocognitive deficits, dopamine dysregulation, and novel applications of mindfulness-based interventions. As our understanding of these conditions evolves, novel diagnostic tools, such as AI-driven screenings and biomarker-based tests, are being developed to facilitate precision medicine approaches. Furthermore, innovative therapies like ketamine infusion, transcranial magnetic stimulation, and personalized nutrition regimens are promising to revolutionize the treatment landscape for those struggling with depression and ADHD.
Important Sources
| Depression or ADHD? How to Differentiate Symptoms - ADDitude | Learn how to recognize signs of depression and ADHD, two common mental health disorders that can co-occur or be comorbid. Find out the differences between primary and secondary depression, manic depression, and how to treat them both with medications and lifestyle changes. |
| The Relationship Between Depression and ADHD - Verywell Mind | Being female: Although ADHD is more common in males, females are more likely to have comorbid ADHD and depression. Inattentive type: Those diagnosed as inattentive type are more likely also to have a diagnosis of depression. Mother's mental health: When a mother has depression during pregnancy, this is linked to a higher likelihood of giving birth to a child who is later diagnosed with ADHD ... |
| The Link Between ADHD and Depression - Verywell Health | Mood: ADHD mood swings are rapid and can be dramatic, while depressive moods tend to be chronic and affect most areas of life. Motivation: People with ADHD may feel initially motivated when presented with a task, but may have difficulty figuring out how to start due to hyperactivity or lack of organizational skills.People with depression often feel hopeless and have no energy to start a task ... |
| ADHD and Depression: Are They Connected? | Psych Central | ADHD and depression are common conditions that share some symptoms, such as low motivation, fatigue, and mood swings. Learn about the possible link between them, the risk factors, and the treatment options from Psych Central, a trusted source of mental health information and resources. |
| Depression and ADHD: How They’re Linked - WebMD | Also, ADHD can lead to depression when people have a hard time with their symptoms. Children may have trouble getting along in school or with playmates, or adults may have issues at work. That can ... |
| ADHD and Depression: What’s the Link? - Healthline | ADHD and depression are both neurodevelopmental disorders that can affect your emotions, behavior, and ways of learning. If you have ADHD, you are more likely to develop depression, and vice versa. Learn the symptoms, risk factors, suicidal thoughts, and treatment options for both conditions. |
| ADHD and Depression: Connection, Risks, Treatment - ADDitude | ADHD and depression are typically treated through psychotherapies, medications, or a combination of the two. Cognitive behavioral therapy (CBT), for instance, has proven to be highly effective against depression. The first goal of CBT is to enable the patient to identify and reduce frequent, intense negative thoughts — “This is too hard to ... |
| ADHD and Depression - Understanding The Connection & Risk - PsyCom | ADHD and/or depression are typically treated with medication and talk therapy.⁸ Psychotherapy, cognitive and behavioral therapy, and psychoeducation can introduce coping skills for symptoms, help build self-esteem, and teach a person to reframe negative thoughts and interrupt destructive behaviors. Children with ADHD and depression may also ... |
| ADHD and depression - Understood | One reason is that ADHD can create a lot of challenges for kids, and those challenges can lead to depression. School and behavior problems can wear down their self-esteem. Trouble with social skills can make them feel isolated. Some people with ADHD may also be “pre-wired” for depression. ADHD involves differences in brain chemistry. |
| Attention-Deficit/Hyperactivity Disorder - National Institute of ... - NIMH | Stress, sleep disorders, anxiety, depression, and other physical conditions or illnesses can cause similar symptoms to those of ADHD. Therefore, a thorough evaluation is necessary to determine the cause of the symptoms. Most children with ADHD receive a diagnosis during the elementary school years. |