Living with ADHD, Depression, and Anxiety: Strategies for Managing Co-Occurring Conditions
Key Takeaways
| Key Takeaways | ADHD | Depression | Anxiety |
|---|---|---|---|
| Symptoms | Difficulty maintaining focus, impulsivity, restlessness | Loss of interest in activities, feelings of sadness, hopelessness | Excessive worry, fear, and nervousness |
| Treatment Options | Methylphenidate, atomoxetine, behavior therapy | Psychotherapy, antidepressant medication, cognitive-behavioral therapy | Therapy, medication, lifestyle changes (exercise, mindfulness) |
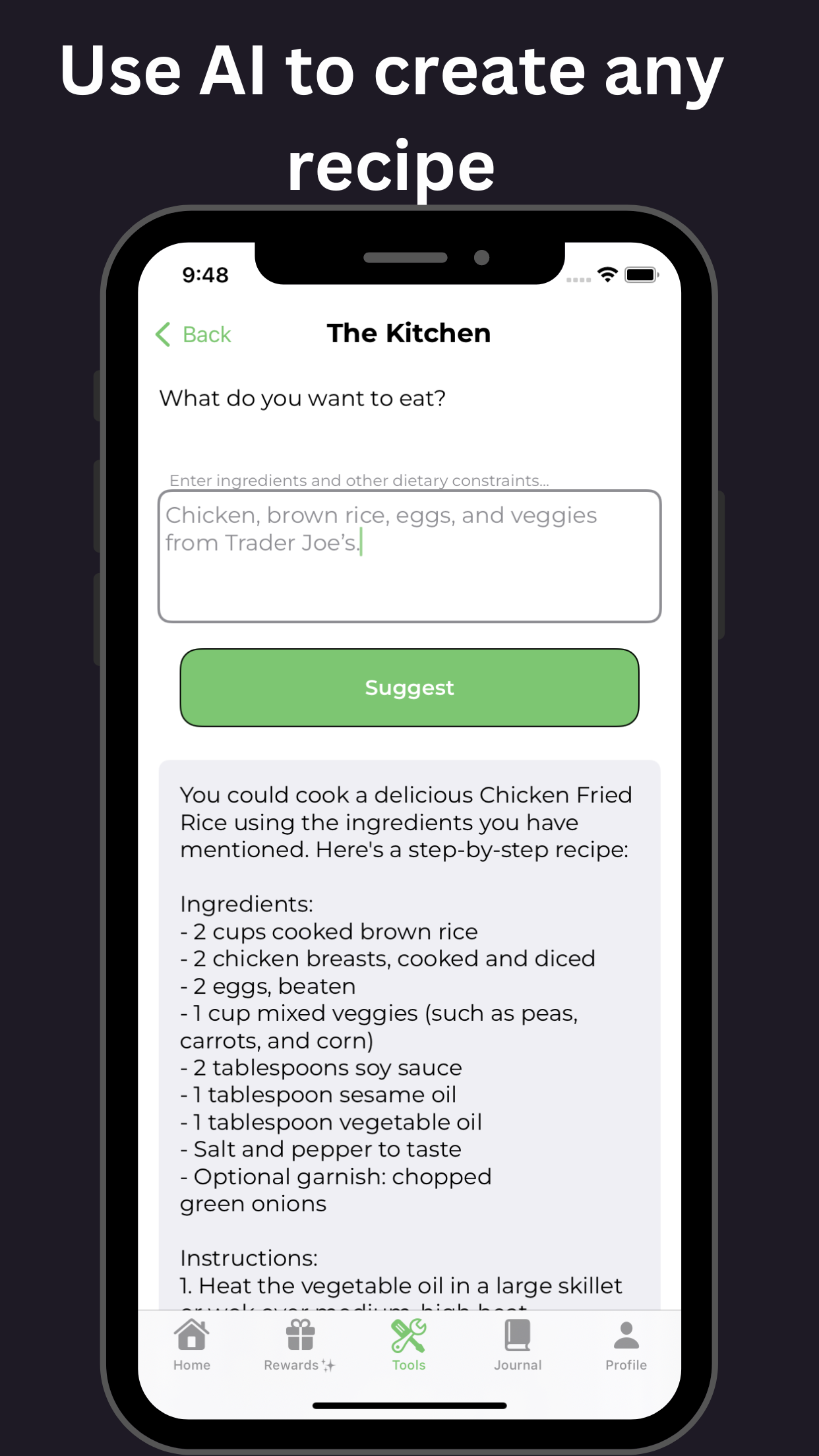
| Dietary Considerations | Omega-3 fatty acids, vitamin D, low-sugar diet | Omega-3 fatty acids, complex carbohydrates, tryptophan-rich foods | Avoid high-sugar, high-caffeine foods; focus on complex carbohydrates and fiber |
| Lifestyle Changes | Regular exercise, structured routine, stress management | Getting enough sleep, engaging in activities that bring joy | Exercise, meditation, healthy sleep habits |
| Tipping Points | Stress, lack of sleep, certain foods | Major life events, loss of a loved one, feeling overwhelmed | Major life changes, genetics, social pressures |
| Comorbidities | Depression, anxiety, substance use disorder | ADHD, anxiety, substance use disorder | Depression, substance use disorder, sleep disorders |
Understanding Comorbidities: Co-Occurring ADHD, Anxiety, and Depression
Living with ADHD, depression, and anxiety can be overwhelming and affect millions of people worldwide. When individuals struggle with multiple conditions simultaneously, it’s known as comorbidity. In this article, we’ll delve into the complexities of co-occurring ADHD, depression, and anxiety, exploring their symptoms, causes, and treatment options.
What are Comorbidities?
Comorbidities refer to the presence of two or more chronic conditions in an individual. In the case of ADHD, depression, and anxiety, comorbidities can significantly impact daily life, relationships, and overall well-being.
Symptoms of Co-Occurring ADHD, Depression, and Anxiety
- Difficulty concentrating and paying attention (ADHD)
- Persistent feelings of sadness, hopelessness, and loss of interest in activities (depression)
- Excessive worry, fear, and anxiety in everyday situations (anxiety)
- Difficulty sleeping, irritability, and mood swings (co-occurring conditions)
Causes of Co-Occurring ADHD, Depression, and Anxiety
Research suggests that genetics, brain chemistry, and environmental factors contribute to the development of comorbid ADHD, depression, and anxiety. Individuals with a family history of mental health conditions may be more likely to experience these conditions.
Treatment Options for Co-Occurring ADHD, Depression, and Anxiety
Effective treatment often involves a combination of therapies, including:
- Medications: Stimulants for ADHD, antidepressants and mood stabilizers for depression, and anxiolytics for anxiety
- Behavioral therapies: Cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and acceptance and commitment therapy (ACT)
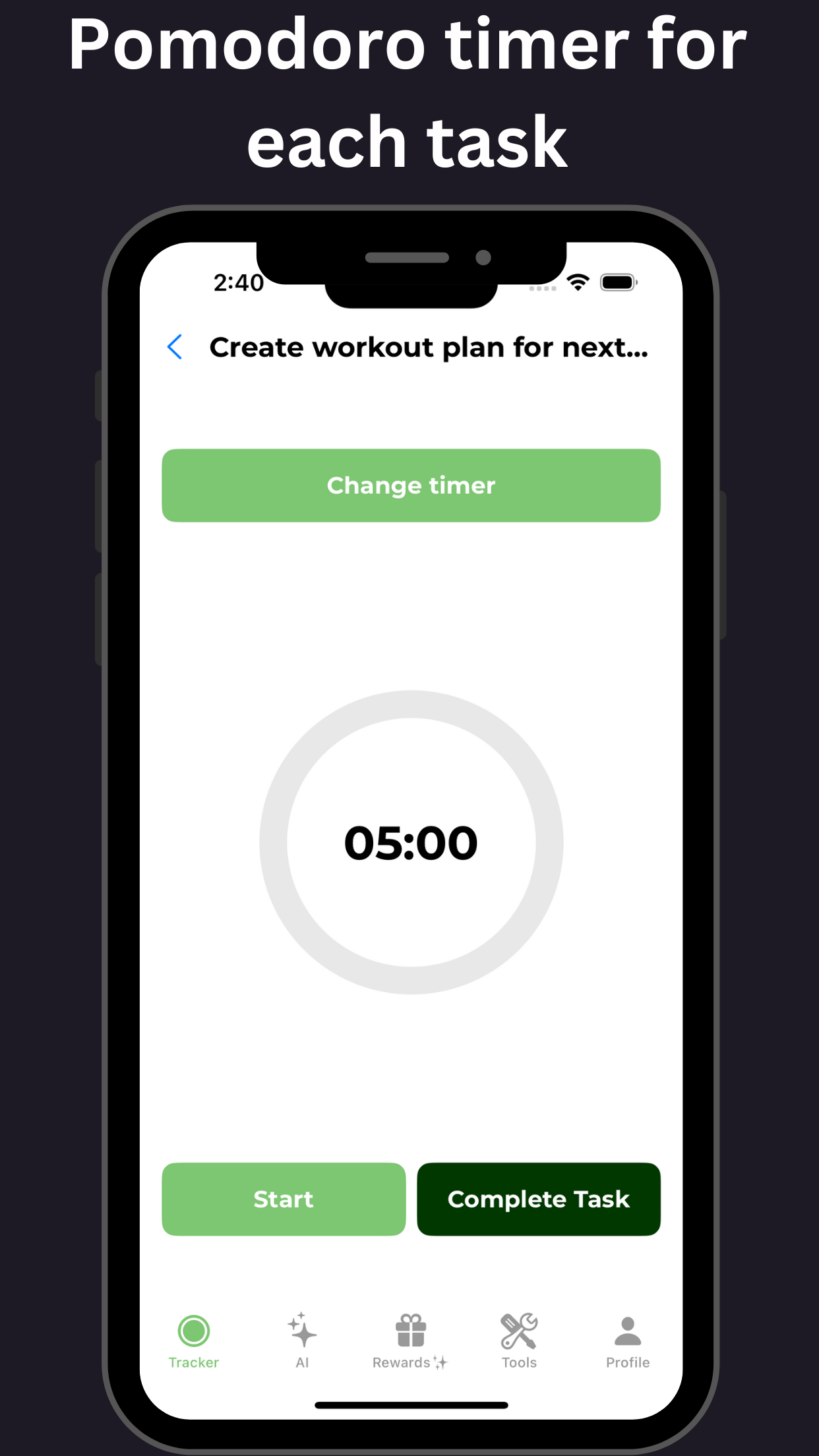
- Lifestyle modifications: Regular exercise, healthy diet, and stress management techniques
Managing Co-Occurring ADHD, Depression, and Anxiety
Managing co-occurring conditions requires a comprehensive approach, including:
- Working with mental health professionals to develop a personalized treatment plan
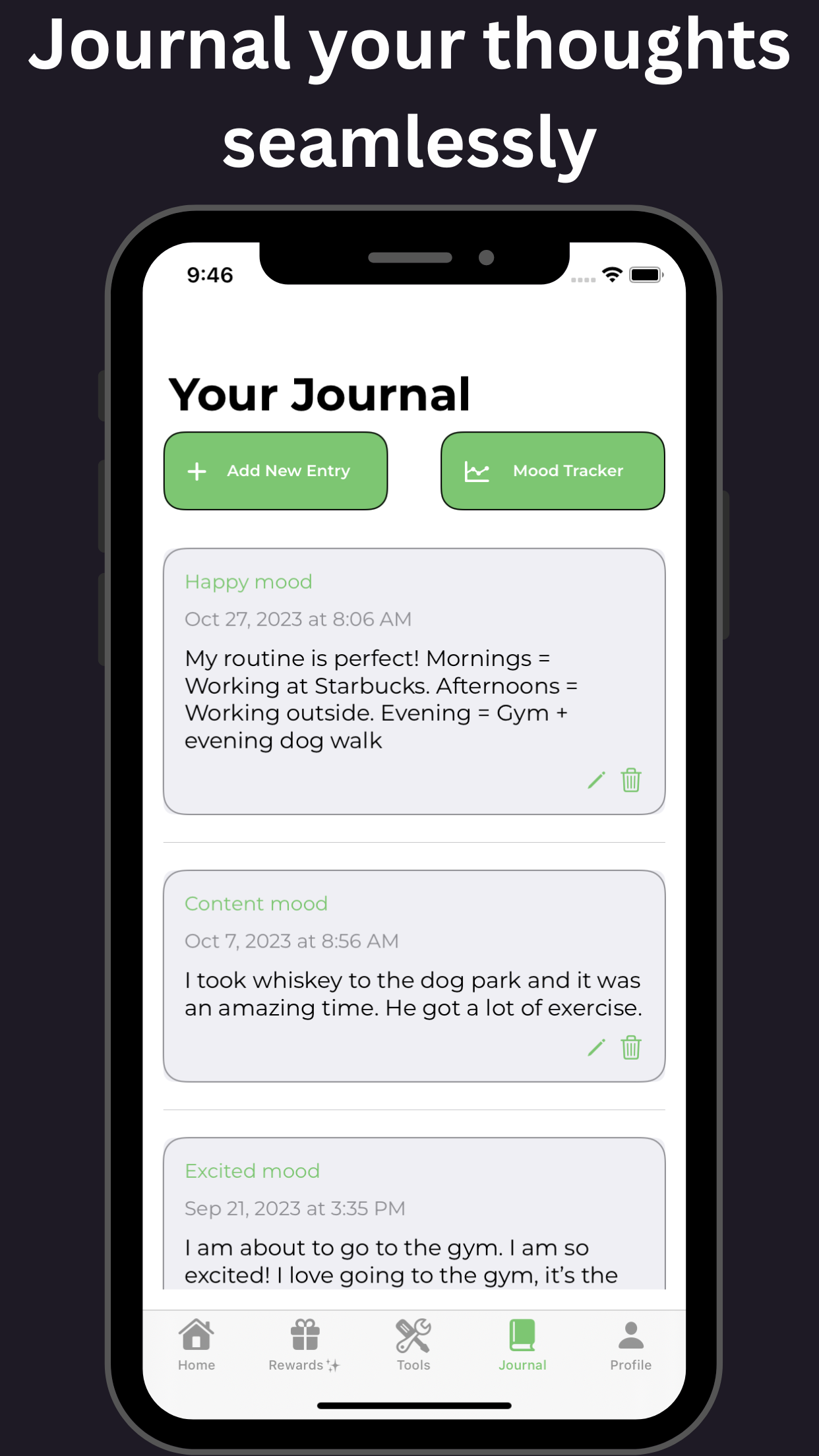
- Practicing self-care and stress management techniques
- Building a support network of family and friends
- Engaging in activities that promote relaxation and enjoyment
Conclusion
Co-occurring ADHD, depression, and anxiety can be challenging to navigate, but it’s essential to address these conditions simultaneously for effective treatment. By understanding the causes, symptoms, and treatment options, individuals can take the first step towards managing their co-occurring conditions and improving their overall well-being.

The Correlation Between ADHD, Depression, and Anxiety: Causes and Consequences
Attention Deficit Hyperactivity Disorder (ADHD), depression, and anxiety are three distinct yet interconnected mental health conditions that can affect millions of individuals worldwide. The relationship between these conditions is complex, with each influencing the others in various ways. In this section, we will delve into the causes and consequences of the correlation between ADHD, depression, and anxiety, exploring the challenges of treating these co-occurring conditions and offering hope for those seeking relief.
Causes of the Correlation:
- Shared Genetic Predisposition: Individuals with a family history of mental health conditions are more likely to experience co-occurring issues.
- Neurobiological Overlap: Overlapping brain regions and neurotransmitter systems in these conditions highlight the intricate relationship.
- Environmental and Trauma Factors: Exposure to adverse childhood experiences can increase the risk of developing multiple conditions.
Consequences of the Correlation:
- Pervasive and Interfering Symptoms: Exacerbated conditions lead to a decline in overall mental health and quality of life.
- Difficulty with Diagnosis and Treatment: Challenges due to the complexity of symptoms necessitate comprehensive treatment plans.
- Increased Risk of Substance Abuse and Other Comorbidities: Co-occurrence raises the likelihood of substance abuse and additional mental health issues.
Breaking the Cycle: Strategies for Overcoming Co-Occurring ADHD, Depression, and Anxiety
To effectively manage these conditions, a multidisciplinary approach that incorporates the following is essential:
- Comprehensive Diagnostic Evaluation: Assessments by qualified healthcare professionals are crucial.
- Medication Management: Alleviate symptoms through a combination of medications and therapies.
- Behavioral Therapies: Interventions help individuals manage symptoms and improve relationships.
- Lifestyle Changes: Promote responses through regular exercise, healthy eating, and stress management.
Conclusion
The correlation between these conditions requires a collaborative approach to treatment. By understanding the multifaceted interplay of ADHD, depression, and anxiety, individuals can work towards reclaiming their mental health and well-being.
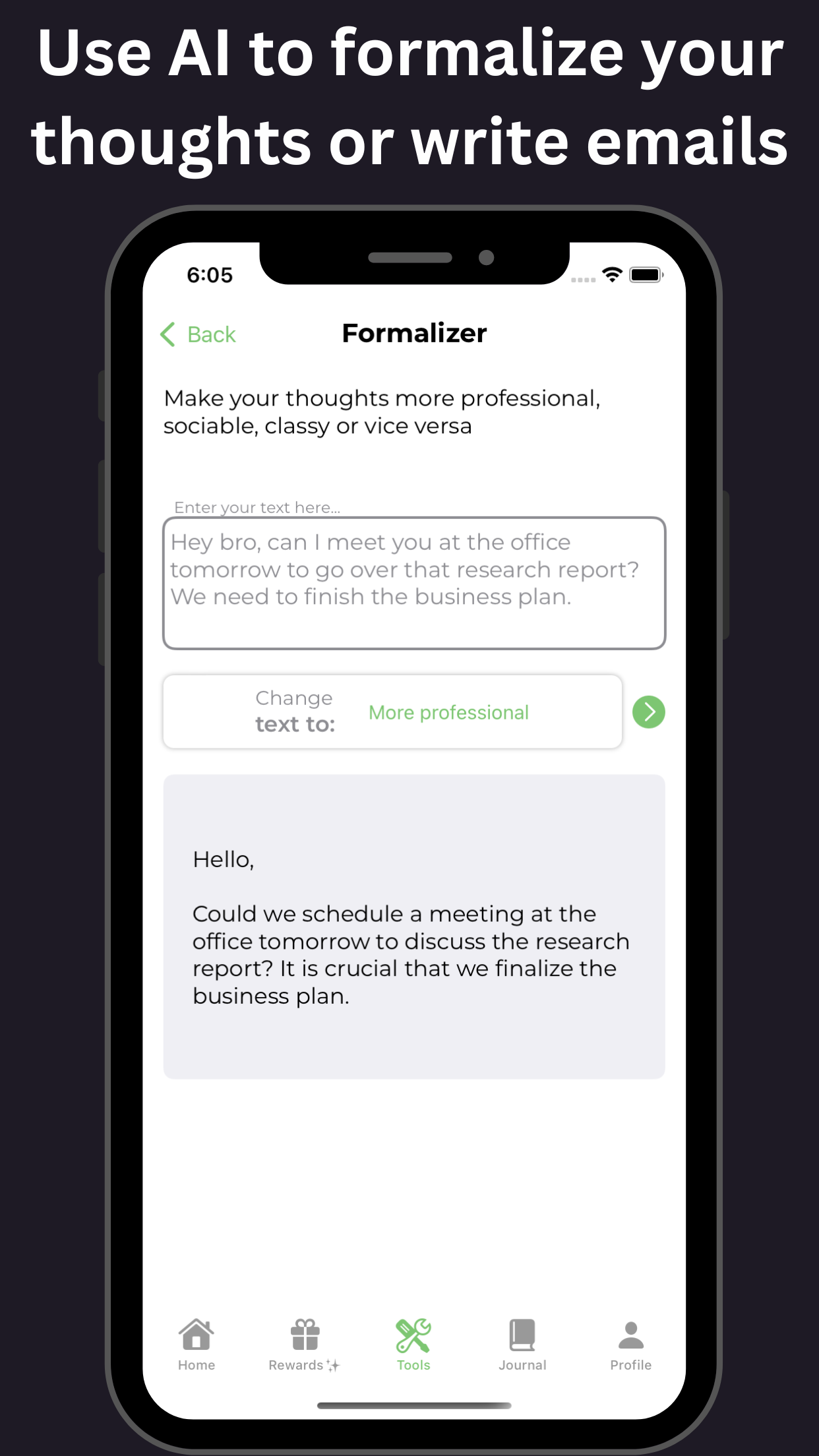
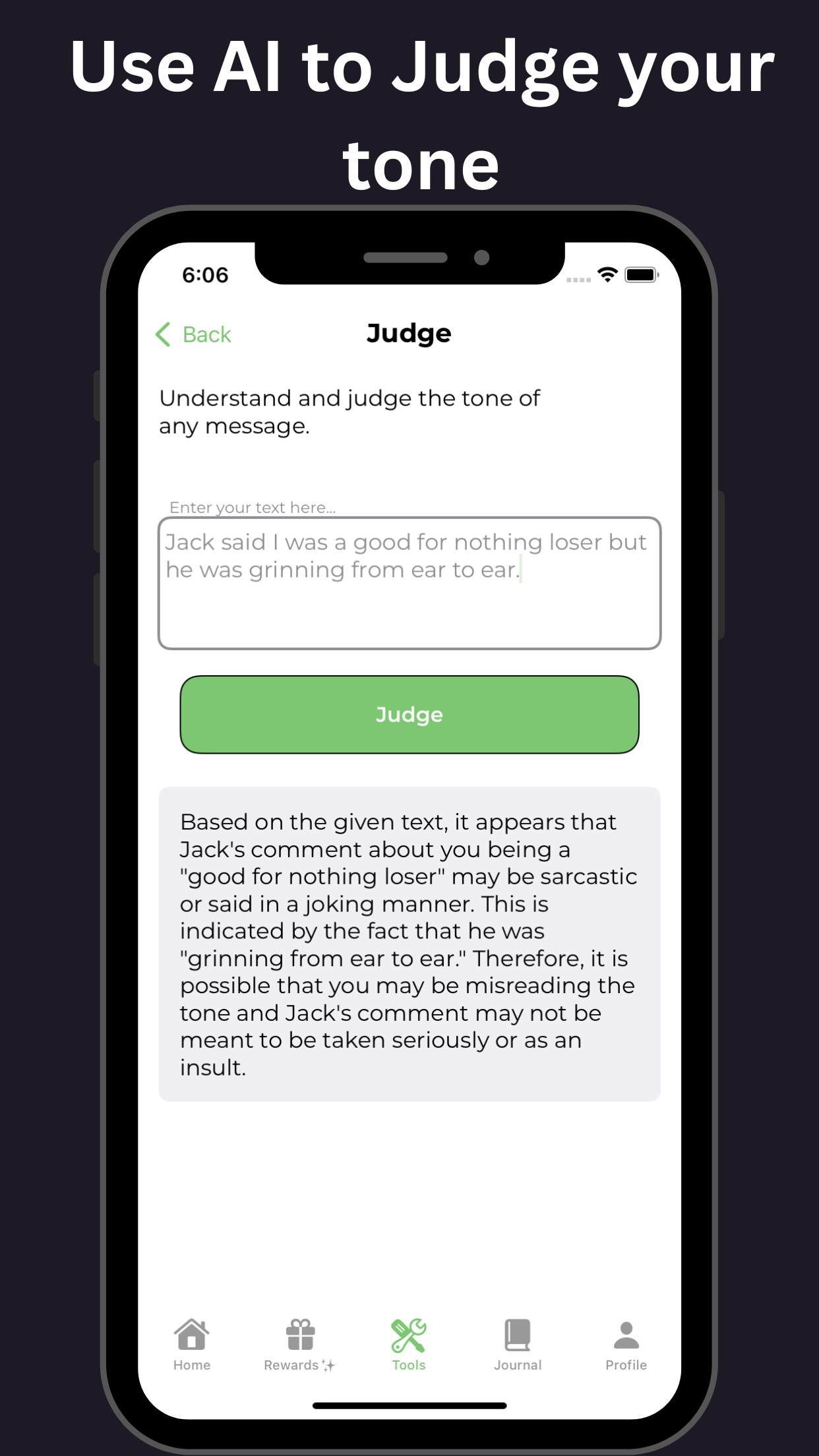
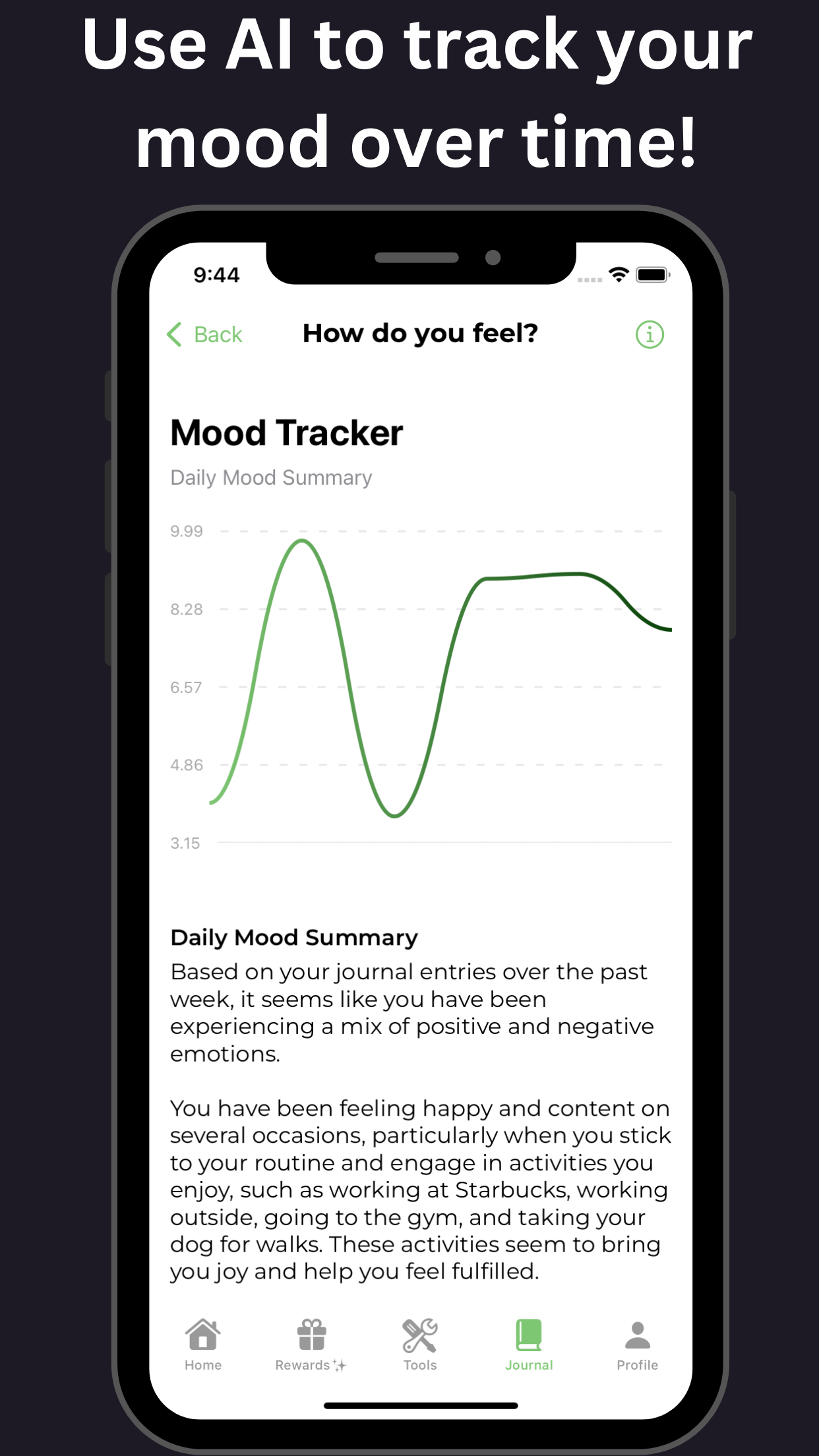
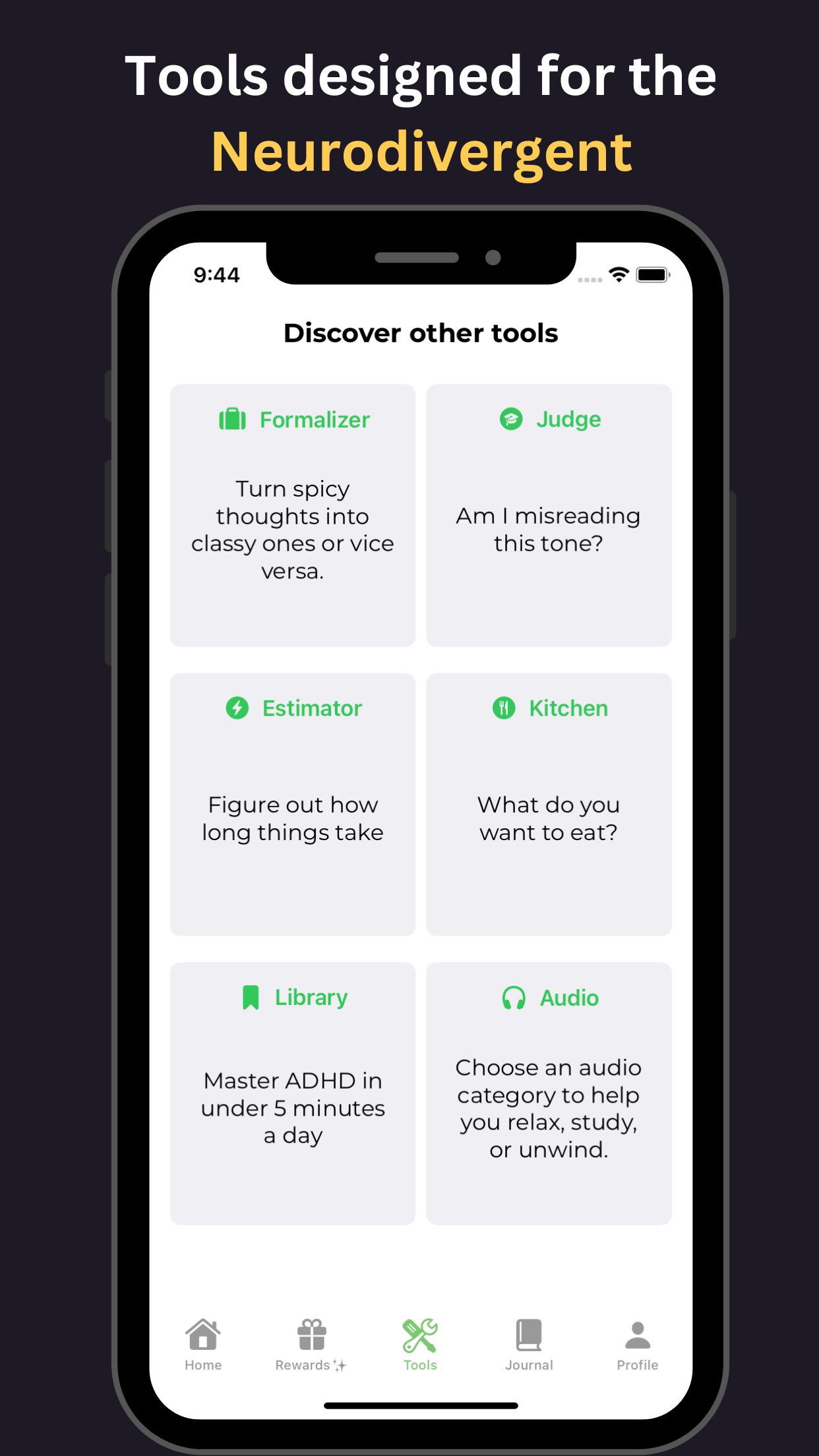
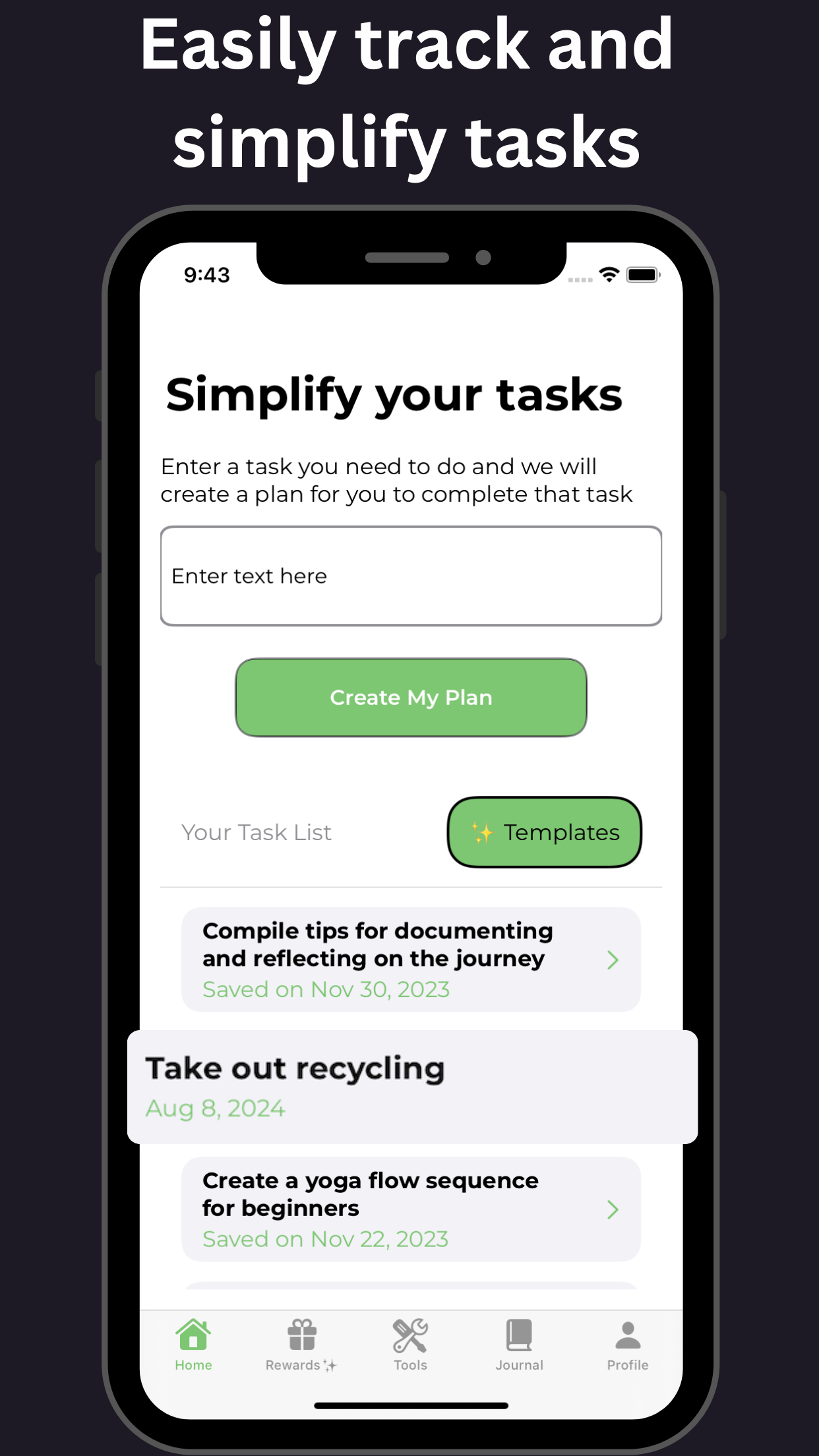
Utilizing tools available through GoblinX, individuals can access various support mechanisms designed for anxiety and ADHD management.
For more resources and tools, visit the GoblinX Website.
The Link Between ADHD, Anxiety, and Depression: Overlapping Symptoms and Risk Factors
For individuals living with ADHD, the risk of developing comorbid conditions such as depression and anxiety is significantly higher. Research suggests that nearly 70% of adults with ADHD will experience a mood disorder, emphasizing the need to explore the link between these conditions.
The Shared Risk Factors:
- Genetic predisposition: A family history of these disorders increases the likelihood of developing them.
- Brain structure and function: Abnormalities may impact emotional regulation and attention.
- Environmental factors: Trauma and stress can raise risks for these conditions.
The Relationship Between Depression and ADHD: Factors Influencing Diagnosis and Treatment
Living with ADHD alongside depression and anxiety presents additional challenges. Studies indicate that up to 60% of individuals with ADHD may also experience depression.
Factors Influencing Diagnosis:
- Co-occurring symptoms: Overlap can complicate accurate diagnosis.
- Comorbid mental health conditions: Other disorders can interfere with identification and treatment.
- Lack of standardized assessment tools: Diverse treatment outcomes can arise from insufficient diagnostic tools.
- Inadequate training for healthcare providers: This can limit effective diagnosis and management.
Factors Influencing Treatment:
- Multimodal treatment: Effective management often combines therapies and interventions.
- Personalized treatment plans: Tailoring treatments to individual needs is crucial.
- Regular monitoring and follow-up: Ongoing assessments enable effective adjustments.
- Collaboration with mental health professionals: This enhances comprehension of individual needs.
Breaking Down the Stigma and Seeking Help
Seeking help remains the first step toward recovery, addressing the stigma surrounding these conditions.
ADHD, Depression, and Anxiety in Women: Unique Challenges
Women may face different challenges with these conditions, including societal expectations and reproductive cycle changes that can exacerbate symptoms.
An Introduction to Inattentive Type ADHD: Comorbidities and Depression
Inattentive Type ADHD often co-occurs with various mental health conditions, especially depression.
The risk factors for depression include genetic predisposition and environmental challenges faced by individuals with ADHD.
Additional Information and Support
For anyone grappling with ADHD, depression, and anxiety, exploring the support offered by GoblinX can provide resources tailored to your needs.
Important Sources
| Comorbidities: ADHD, Anxiety, Depression - ADDitude | The ADHD affects the comorbid disorder and, in turn, is affected by depression or anxiety. |
| The Correlation Between ADHD, Depression, And Anxiety | Individuals may experience comorbid symptoms. |
| Understanding the link between ADHD, anxiety and depression | Learn how ADHD, anxiety and depression can coexist. |
| The Relationship Between Depression and ADHD - Verywell Mind | Mood swings and motivation issues often overlap with these conditions. |
| Depression and ADHD: How They’re Linked - WebMD | Discover the mutual impact of ADHD and depression. |
| The Link Between ADHD and Depression - Verywell Health | ADHD and depression can deeply affect overall quality of life. |
| ADHD and Depression: Are They Connected? | Psych Central | Explore the connections between ADHD and repeated mood episodes. |
| Relationship Between ADHD and Anxiety - Healthline | How these disorders interact with daily functioning. |