Double Diagnosis: Navigating the Complex Relationship Between ADHD, Anxiety, and Depression
Key Takeaways
| Key Takeaways | Description |
|---|---|
| Comorbidity | ADHD often co-occurs with anxiety and depression, with studies suggesting 30-60% of individuals with ADHD also experience anxiety and/or depression. |
| Symptom Overlap | ADHD, anxiety, and depression share similar symptoms, such as difficulty concentrating, restlessness, and mood disturbances, making diagnosis and treatment challenging. |
| Executive Function Deficits | Individuals with ADHD often experience executive function deficits, which can contribute to anxiety and depression by impairing planning, organization, and self-regulation. |
| Neurobiological Factors | Imbalances in neurotransmitters, such as dopamine and serotonin, and altered brain structure and function contribute to the development of ADHD, anxiety, and depression. |
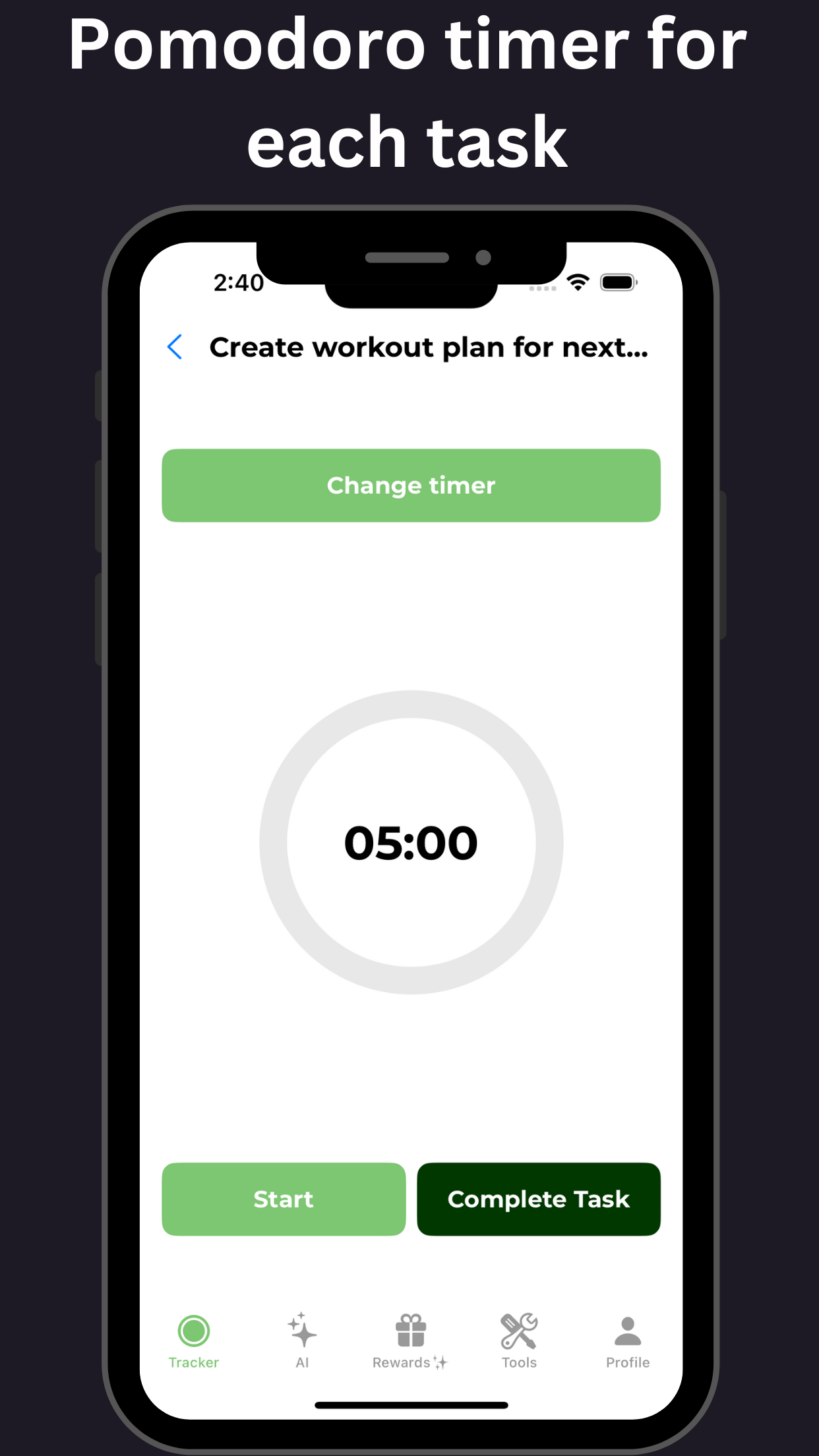
| Treatment Considerations | Treatment for ADHD, anxiety, and depression often involves a combination of medications, behavioral therapies, and lifestyle changes, such as exercise and mindfulness. |
| Medication Interactions | Certain medications used to treat ADHD, such as stimulants, can exacerbate anxiety and depression, while others, such as SSRIs, can help alleviate symptoms. |
The Coexistence of ADHD, Anxiety, and Depression: Understanding how these conditions overlap and affect quality of life
Unlocking the Interconnected World of ADHD, Anxiety, and Depression
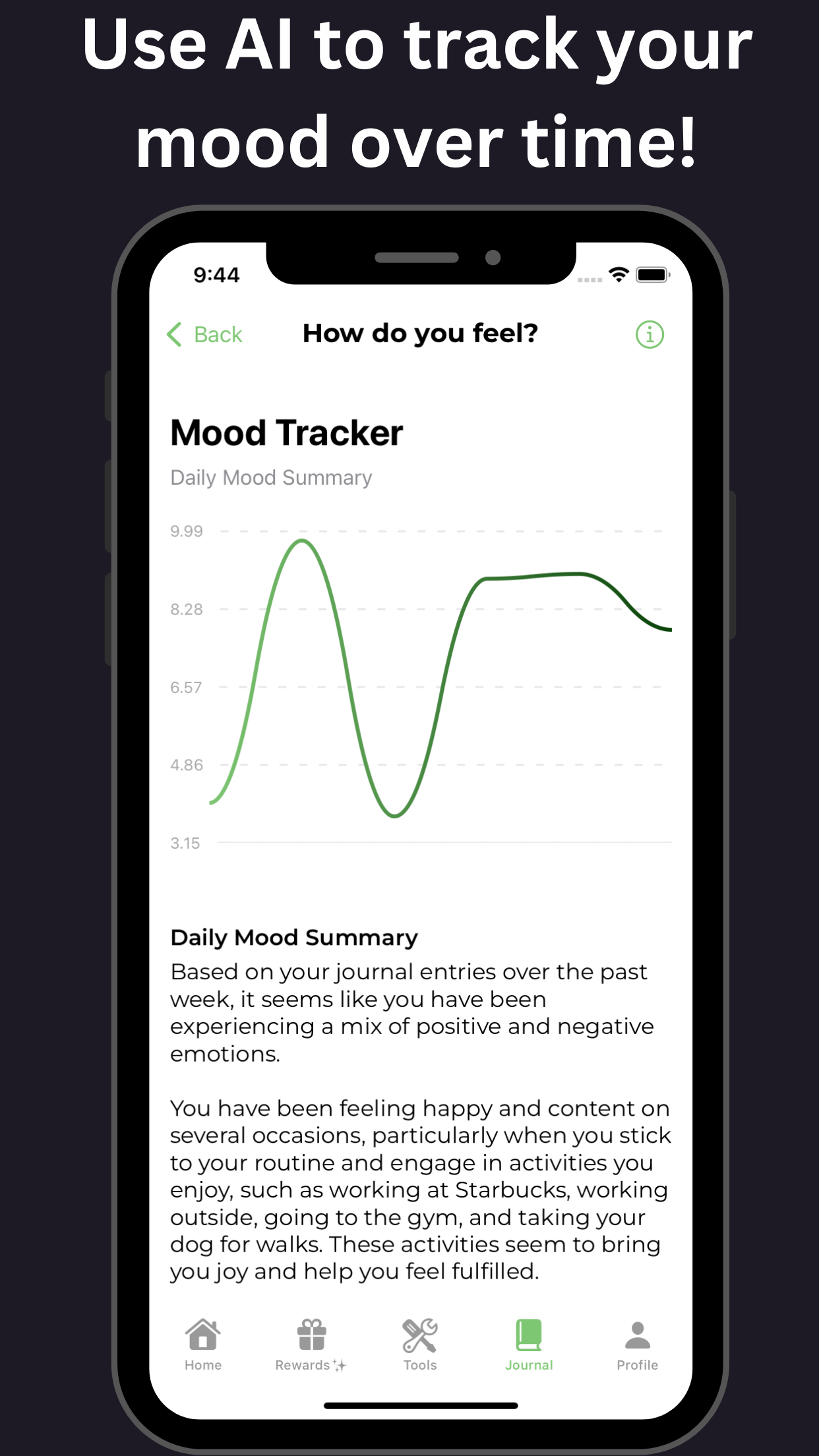
ADHD, anxiety, and depression often coexist, impacting daily life in profound ways. Comorbidities among these conditions affect 60-80% of ADHD patients. ADHD amplifies feelings of frustration and often triggers feelings of worthlessness commonly found in co-occurring anxiety and depression. Shared brain pathways play a pivotal role.
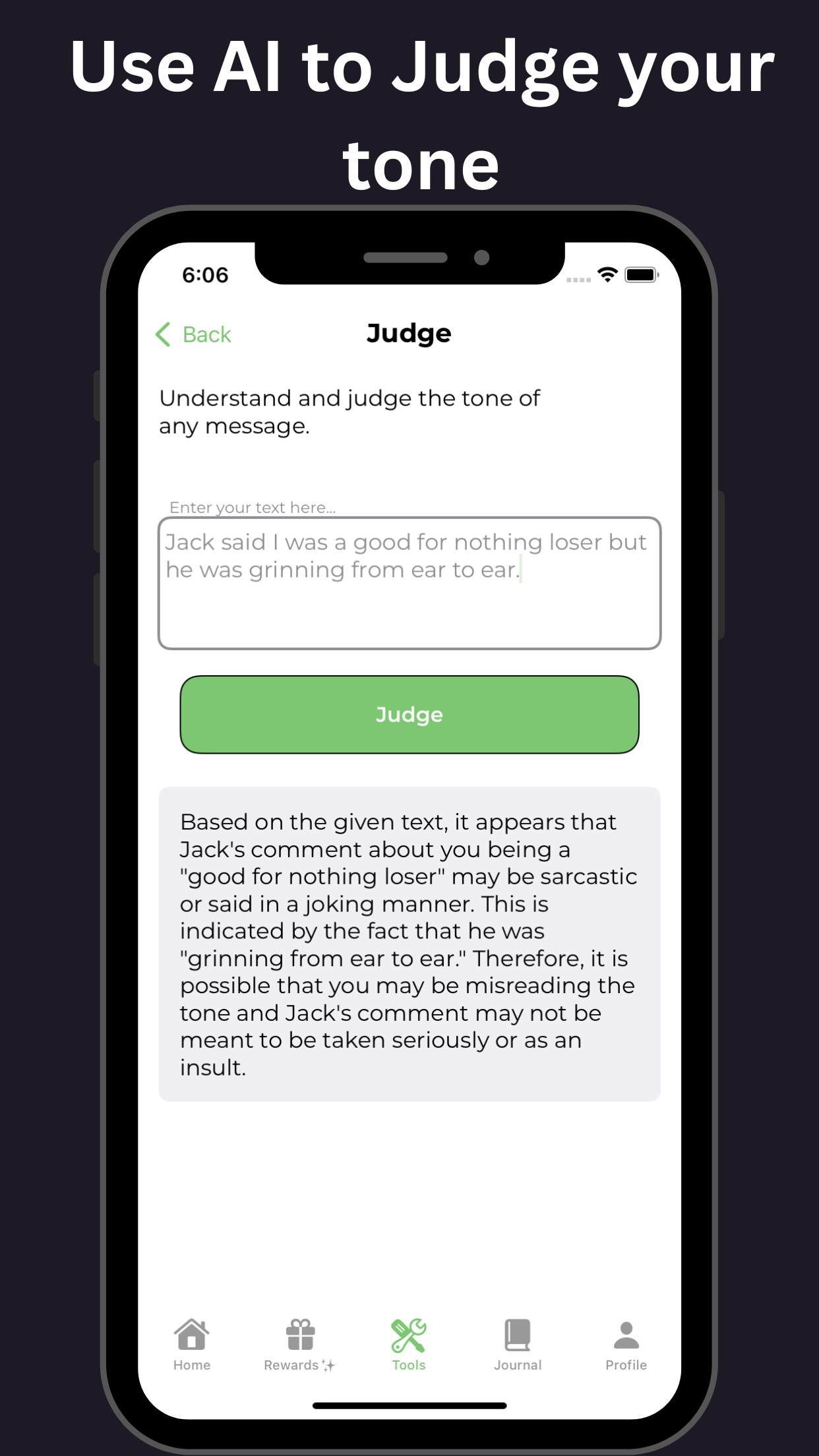
Characterized by concentration and emotional fluctuations, emotional difficulty often reported arises from feelings of worthlessness and the challenge in distinguishing emotional swings that might go undiagnosed due to the intricate interaction between these disorders. Coping with stress exacerbates symptoms, hindering learning and daily functioning. Lack of patience can lead to feelings of panic, overwhelming those affected, thus complicating relationships and social interactions. Recognizing these overlaps is crucial for effective treatment and support.

Unraveling Comorbidities: The Diagnosis Puzzle of ADHD, Anxiety, and Depression: Recognizing how ADHD, anxiety, and depression intersect and impact one another
Attention Deficit Hyperactivity Disorder (ADHD), anxiety, and depression are complex mental health conditions that often intersect and impact one another. Research suggests that individuals with ADHD are more likely to experience comorbid anxiety and depression, with studies indicating that up to 60% of people with ADHD also have a co-occurring anxiety disorder, and 30% experience depression.
The diagnostic puzzle is challenging to unravel, as symptoms often overlap and masquerade as one another. For instance, the inattention and disorganization characteristic of ADHD can be mistaken for symptoms of depression, while the restlessness and impulsivity of ADHD can be misattributed to anxiety.
Key similarities and differences:
- ADHD and anxiety: Both involve difficulties with emotional regulation, leading to feelings of overwhelm and stress. However, ADHD is characterized by symptoms of inattention, hyperactivity, and impulsivity, while anxiety is marked by excessive worry, fear, and avoidance behaviors.
- ADHD and depression: Both can involve difficulties with motivation, concentration, and pleasurable activities. However, depression is characterized by persistent feelings of sadness, hopelessness, and loss of interest, whereas ADHD is marked by inattention and impulsivity.
- Anxiety and depression: Both conditions involve difficulties with emotional regulation leading to overwhelm and stress, where anxiety is characterized by excessive worry and fear, and depression is marked by chronic sadness.
The importance of accurate diagnosis:
Accurate diagnosis is crucial for developing effective treatment plans that address the unique needs of individuals with these comorbid conditions. A comprehensive diagnostic evaluation should include:
- A thorough medical and psychological history.
- A physical examination to rule out underlying medical conditions.
- A psychological assessment including standardized rating scales and diagnostic interviews.
- A review of symptoms, including severity and impact on daily life.
Treatment strategies:
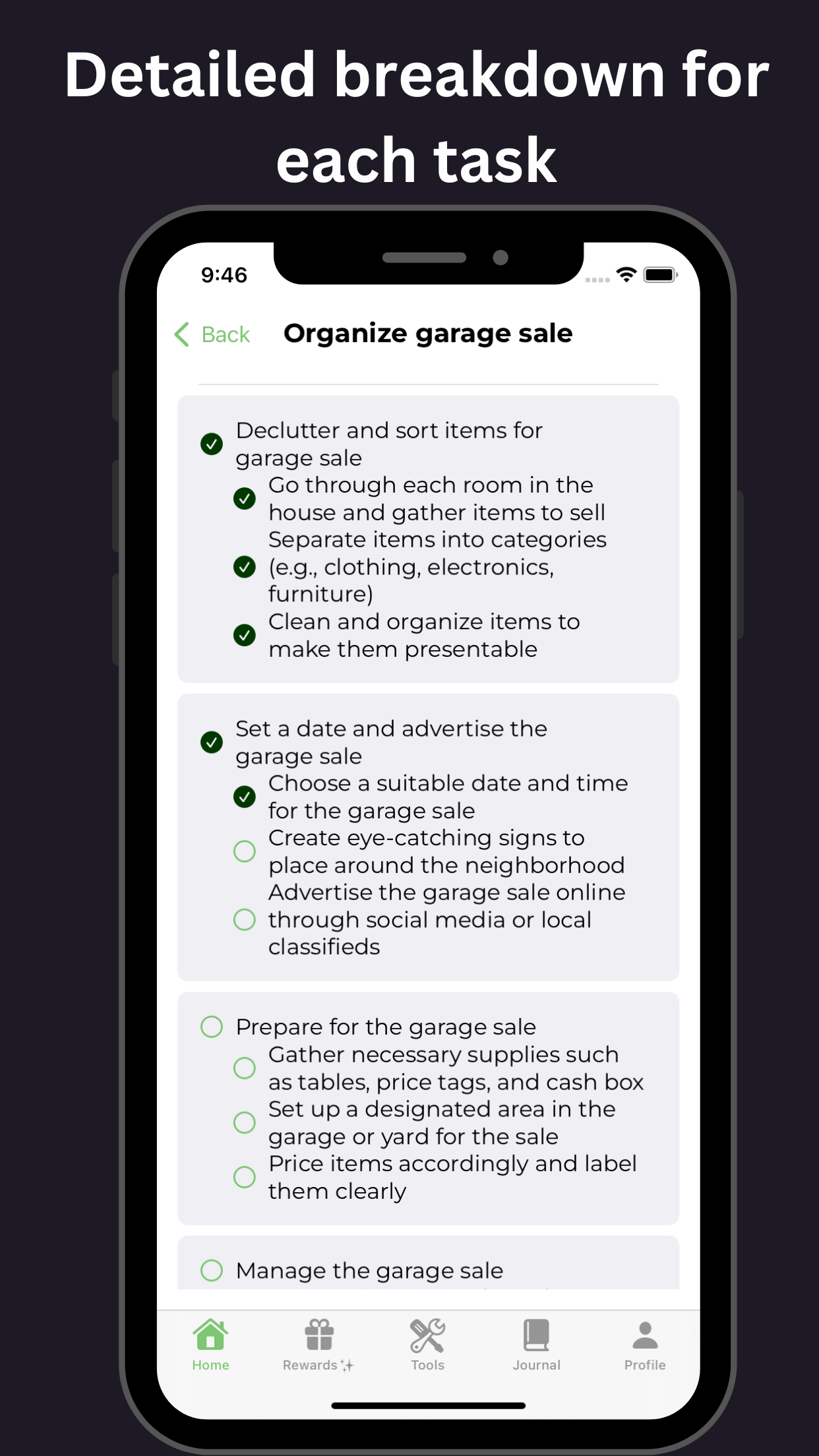
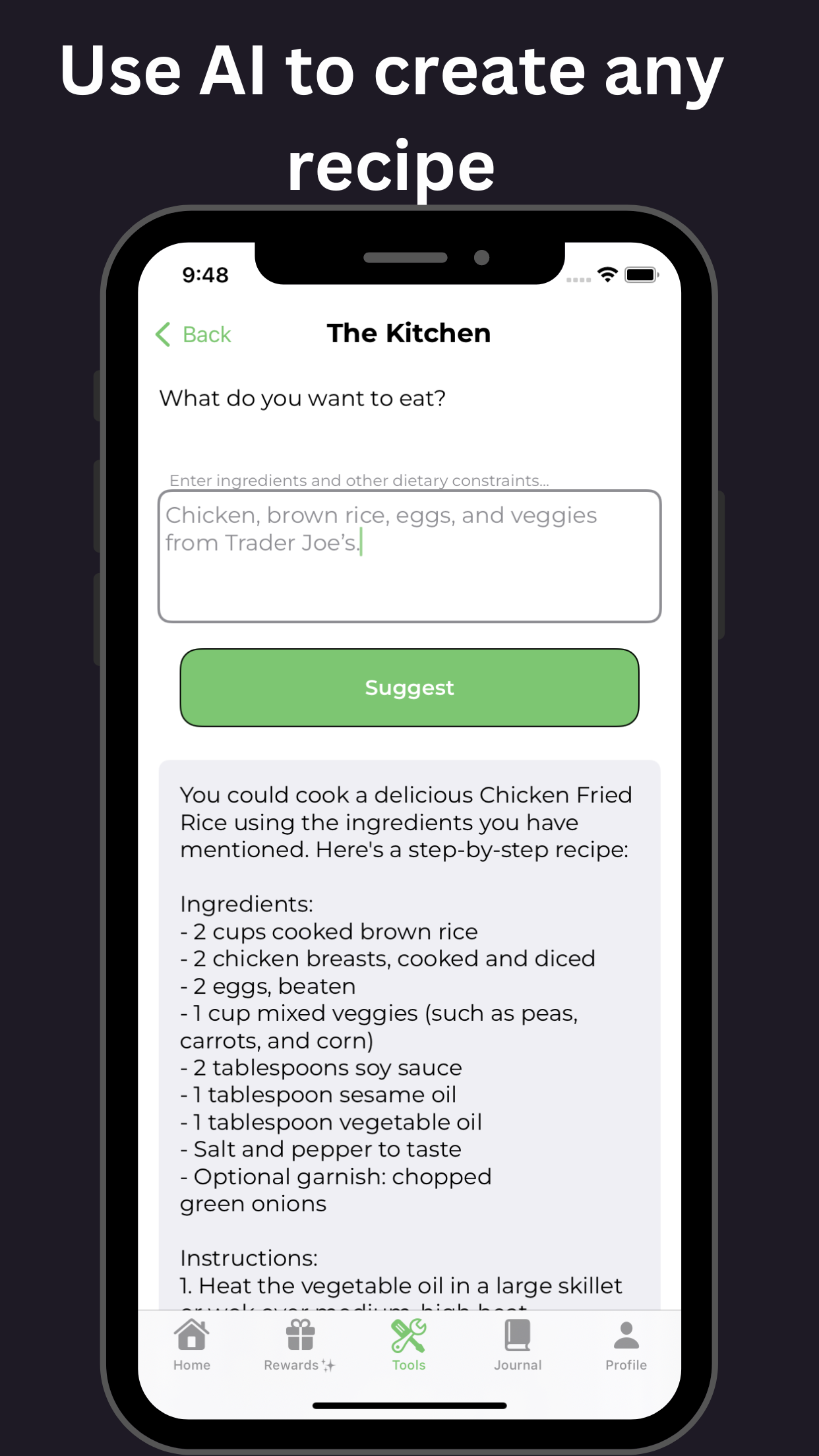
Treatment often involves a combination of medications, behavioral therapies, and lifestyle modifications. Some effective treatment strategies include:
- Medications: Stimulants, non-stimulants, and antidepressants can effectively manage symptoms.
- Behavioral therapies: Cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and mindfulness-based stress reduction (MBSR) can aid in managing symptoms and improving emotional regulation.
- Lifestyle modifications: Regular exercise, healthy sleep habits, and balanced diets can significantly bolster mental well-being.
Conclusion:
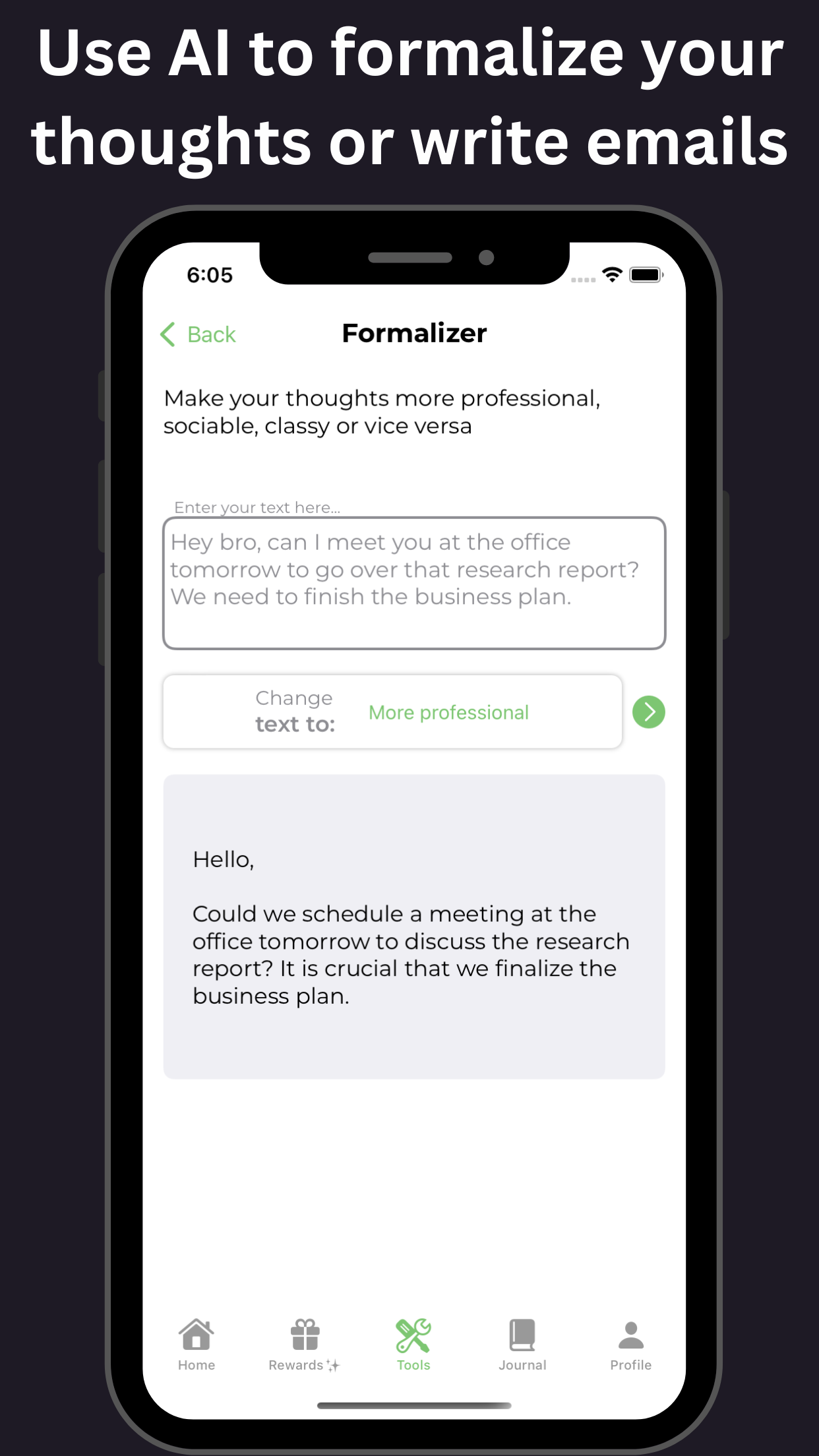
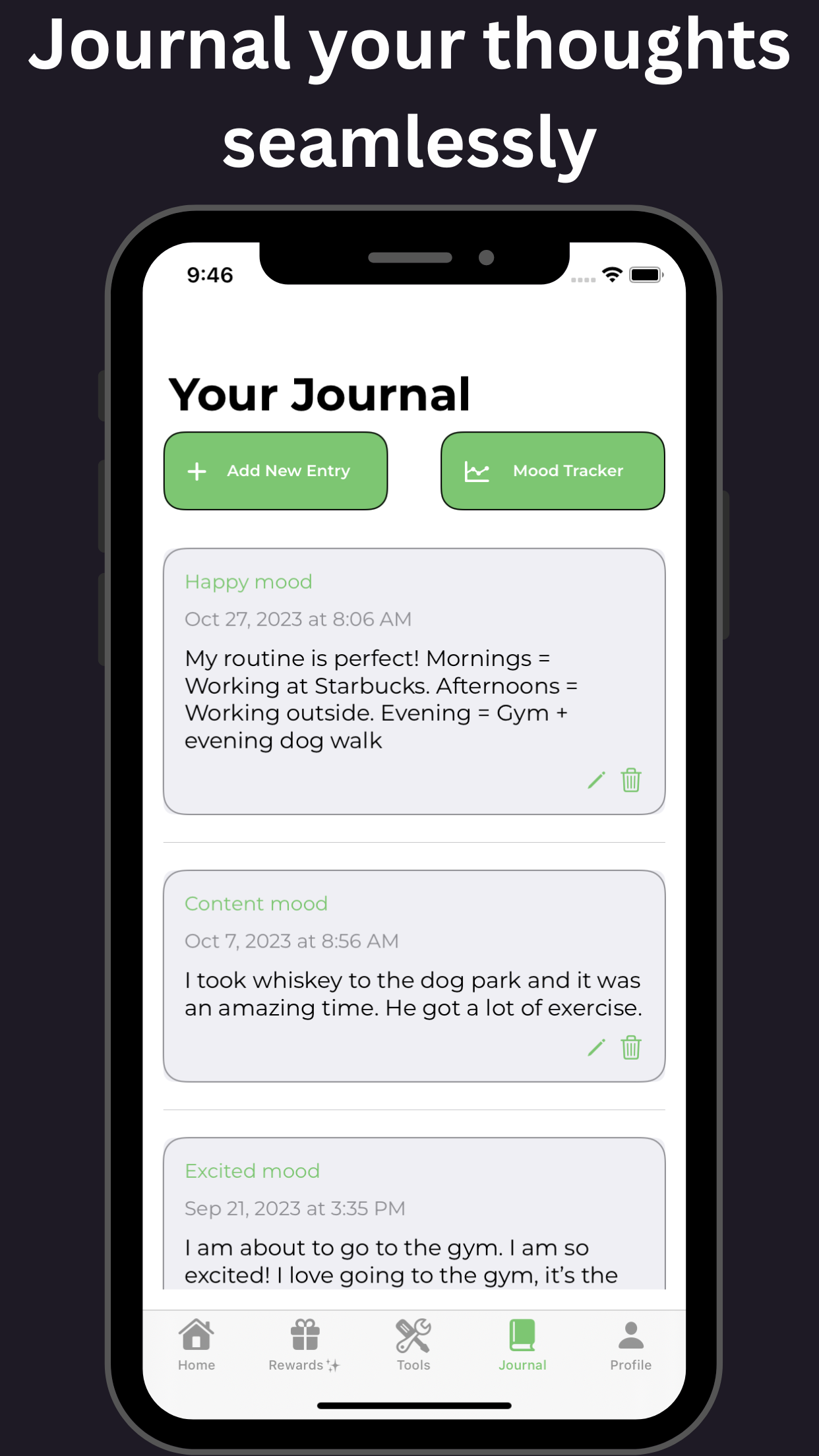
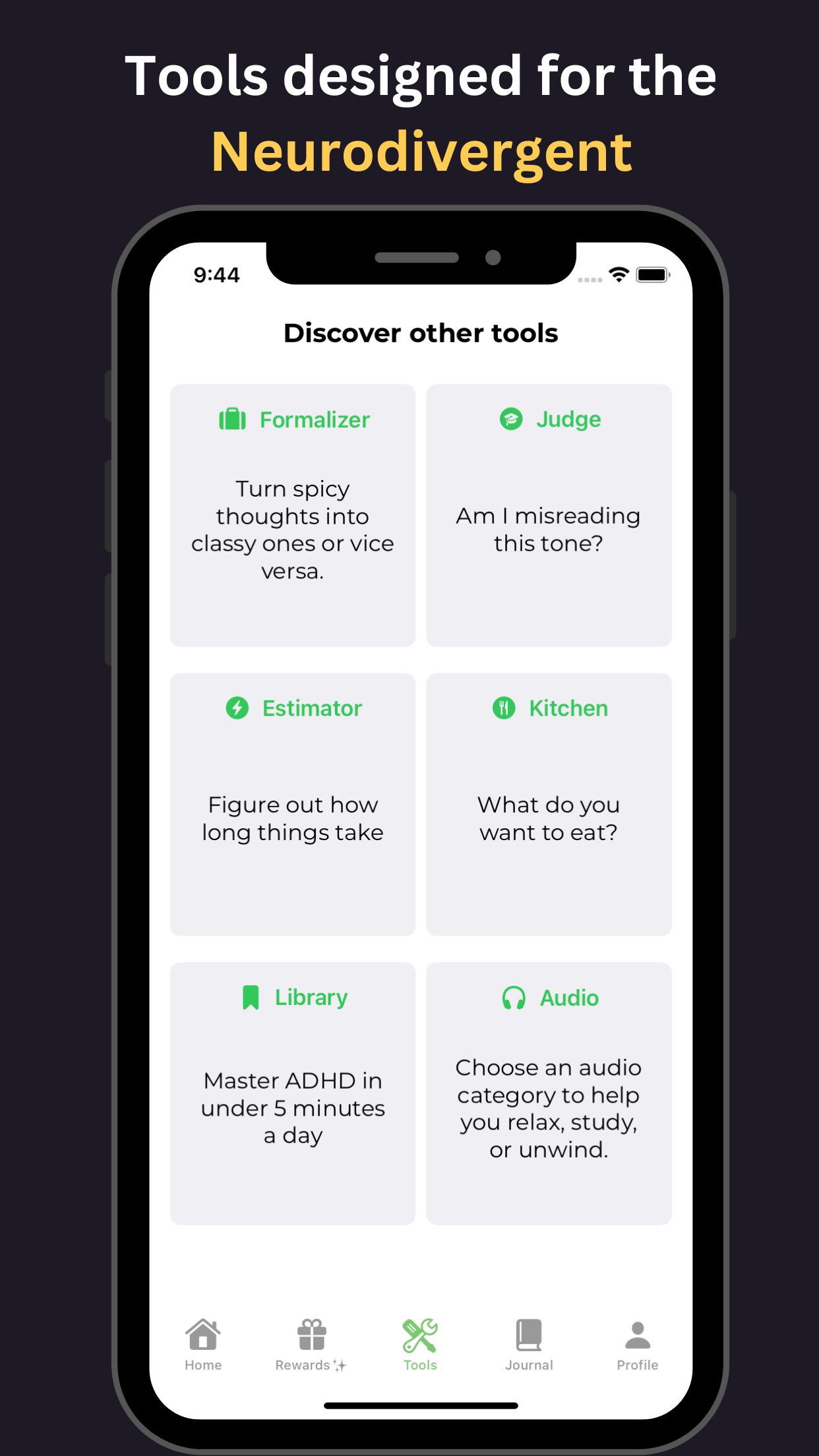
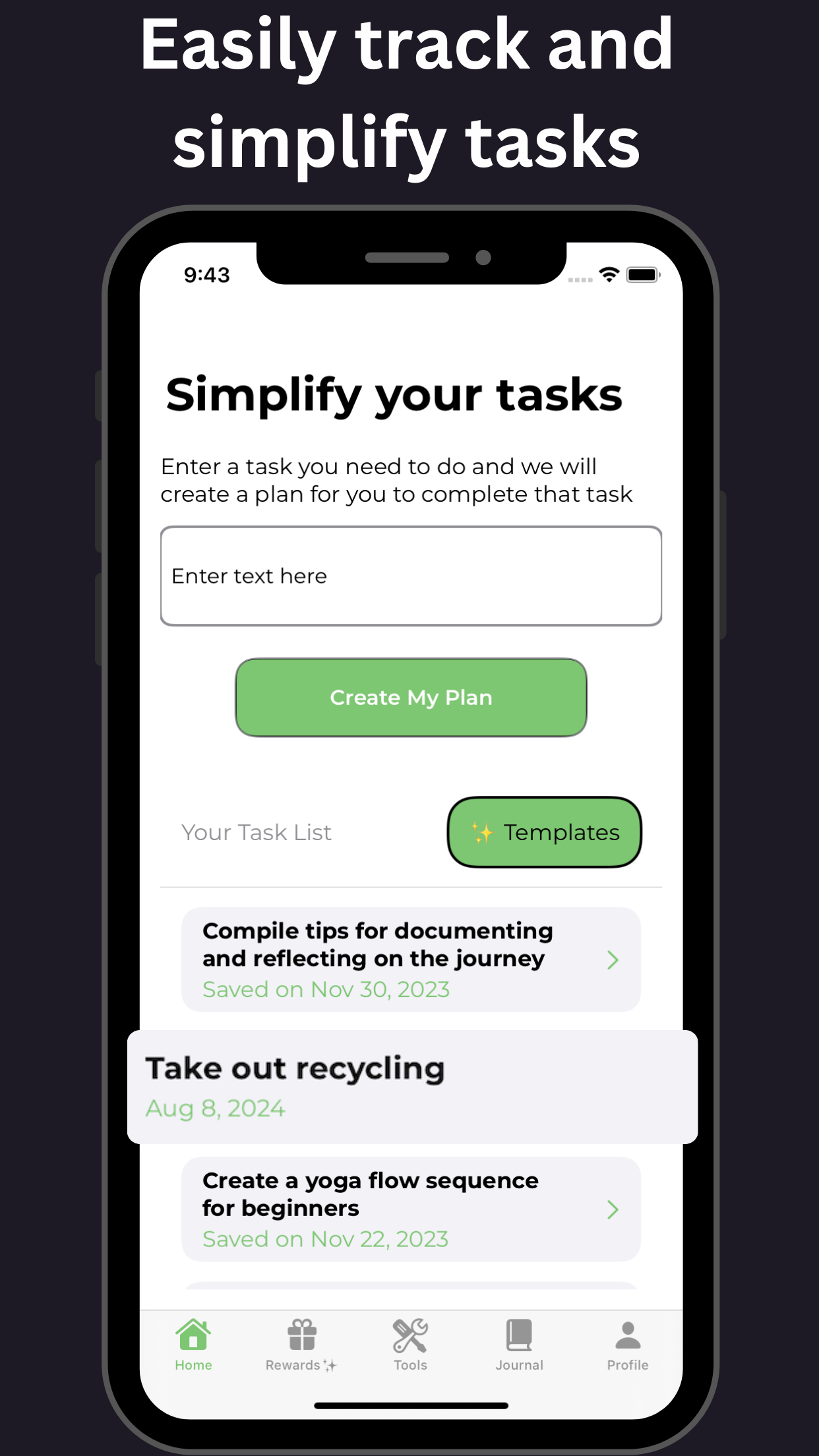
The complex diagnostic puzzle of these conditions can become less daunting through understanding their similarities and differences, leading to accurate diagnoses and effective treatment plans. By addressing individuals' unique needs, we can enhance their quality of life, ideally with tools such as those offered by GoblinX for anxiety and ADHD support.